In today’s complex medical landscape, the significance of efficient communication among healthcare professionals, patients, and their caregivers cannot be overstated. One key instrument that serves this essential role is the Discharge Summary. This critical document outlines a patient’s hospitalization journey, from the initial diagnosis and treatment to the final discharge plan.
The Discharge Summary serves as an essential communication tool bridging the gap between hospital care and community or home-based care. This article delves into the key components of an effective discharge summary, its role in improving patient outcomes, its importance in maintaining continuity of care, and the best practices healthcare providers can adopt to ensure its optimal use.
Table of Contents
What is the Discharge Summary ?

A Discharge Summary is a comprehensive clinical report prepared by healthcare professionals when a patient is discharged from a hospital or other health care settings. It encapsulates the patient’s health history, details of their hospital stay, diagnosis, treatment administered, patient’s condition at discharge, and instructions for follow-up care.
Serving as an essential communication tool, it ensures the continuity of care, facilitates the transition from hospital to home or other care settings, and enhances coordination among healthcare providers, patients, and caregivers.
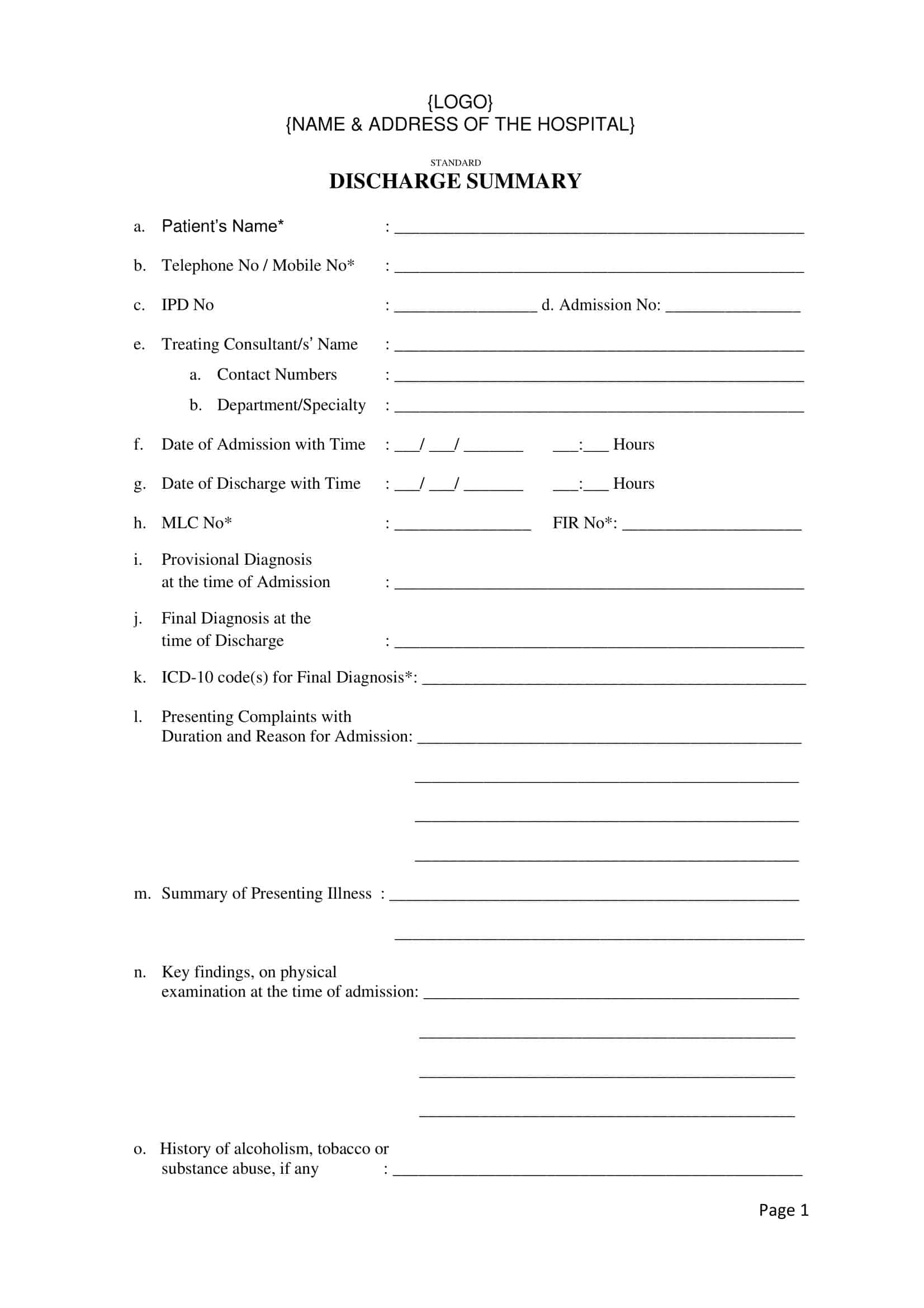
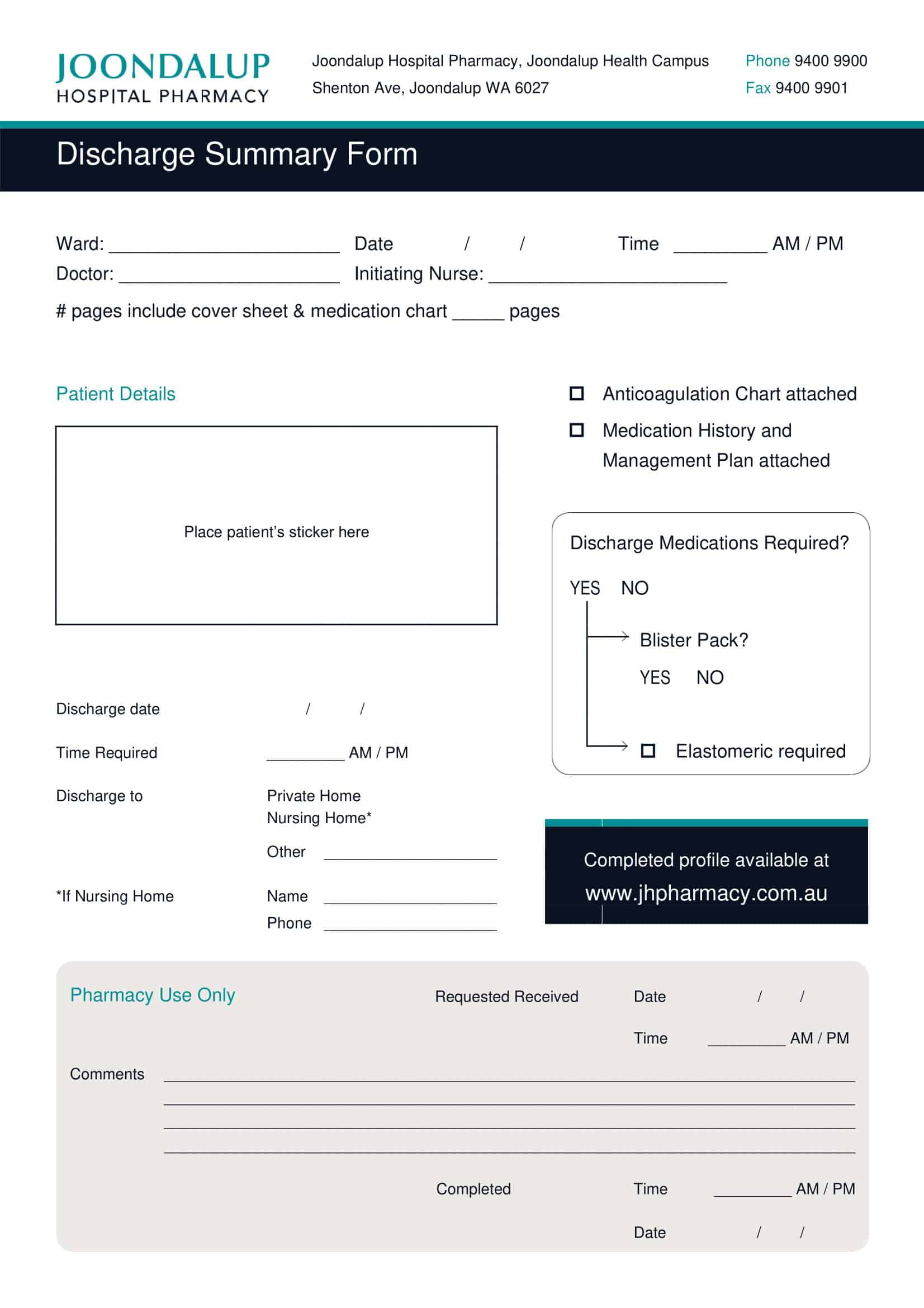
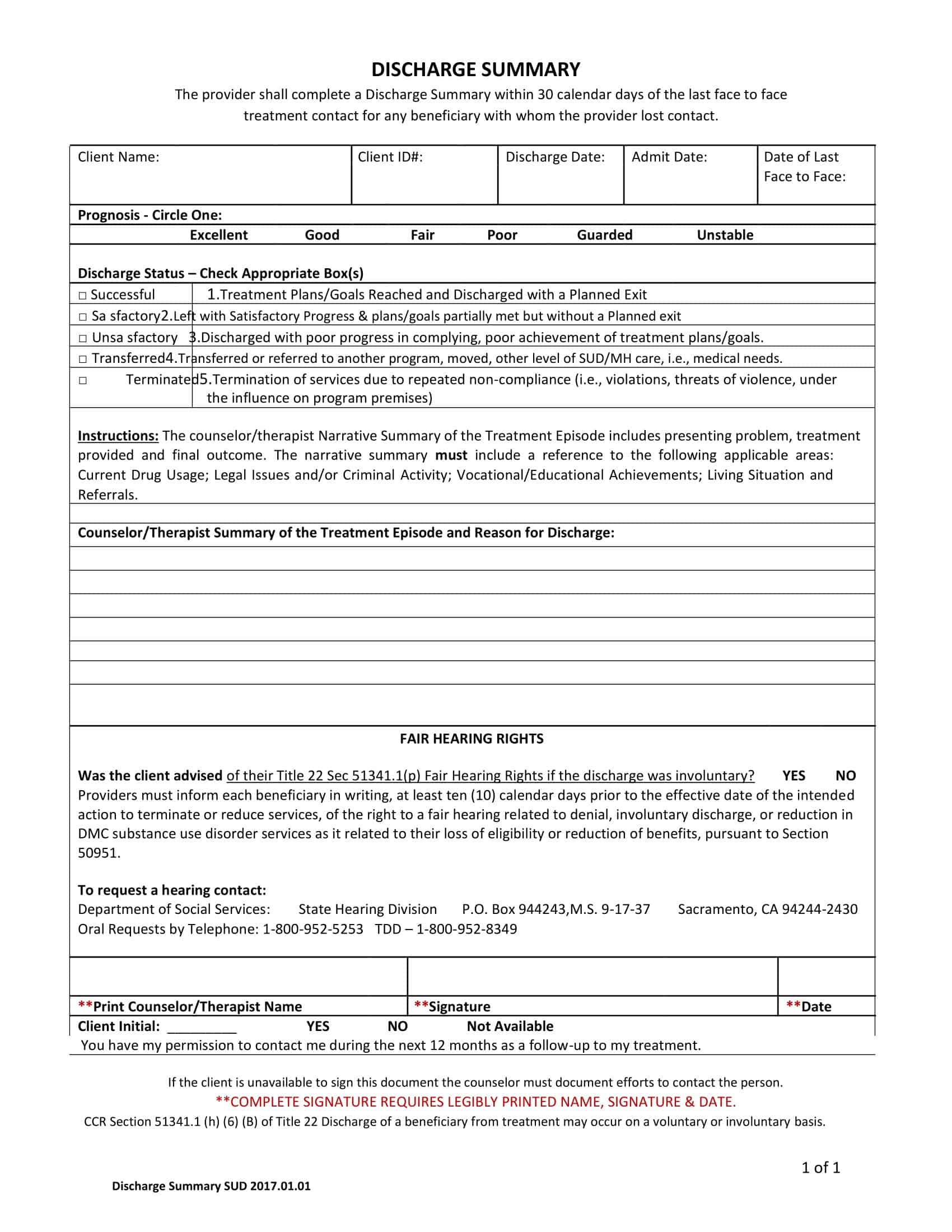
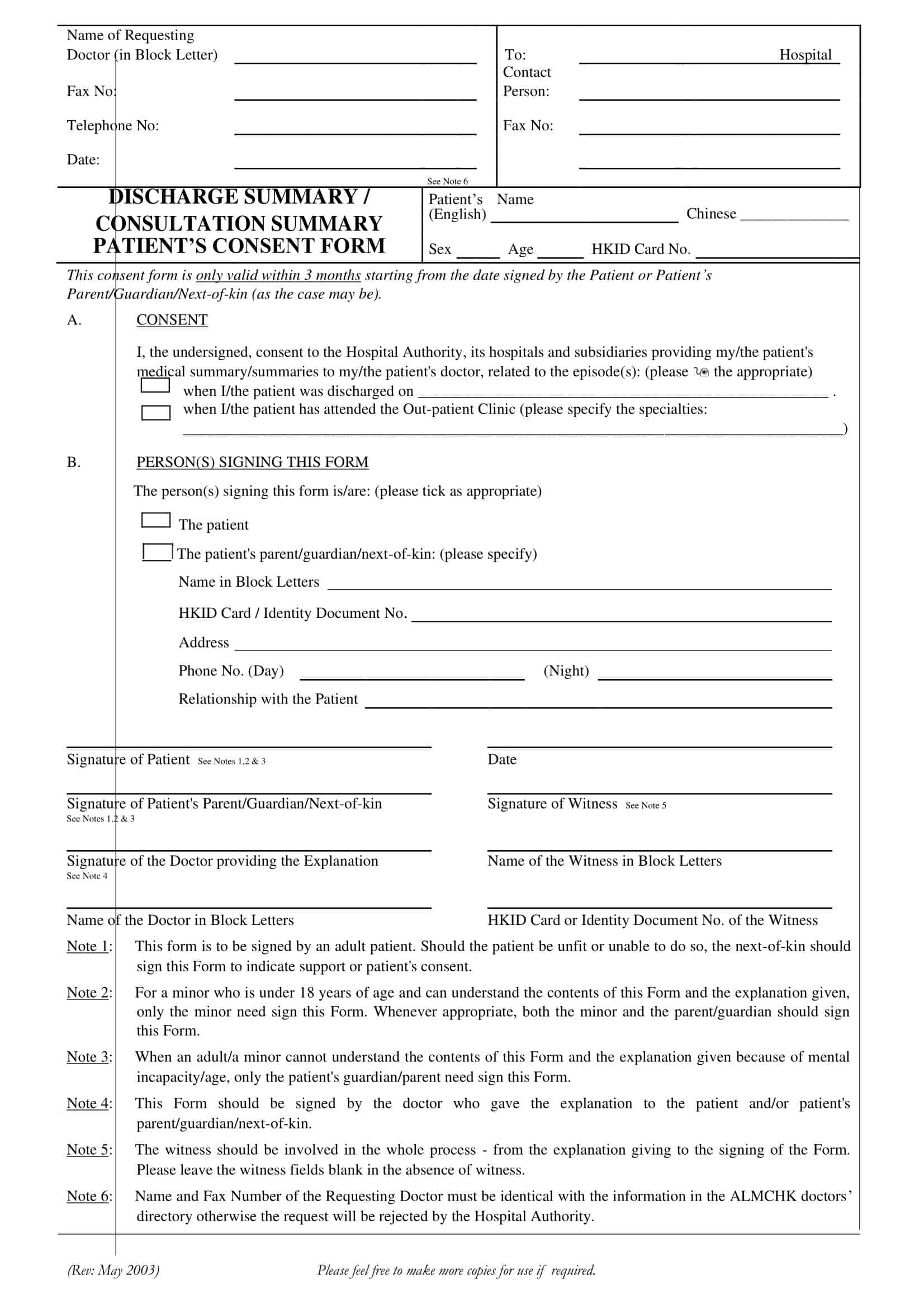
Discharge Summary Templates
Discharge Summary Templates serve a crucial role in healthcare settings, providing a structured format for summarizing a patient’s hospital course and the care received. These templates ensure that healthcare professionals can accurately document all necessary details regarding a patient’s condition, treatment, and future care recommendations upon discharge.
Each template typically contains sections dedicated to critical information such as the patient’s identification details, admission and discharge dates, diagnoses, procedures performed, medication instructions, and follow-up care plans. Many templates also include a space for any relevant notes or observations that the discharging physician or healthcare provider might have.
In a broad range of healthcare scenarios, these templates are indispensable. They are utilized in hospitals, clinics, rehabilitation centers, and other healthcare institutions. Regardless of the patient’s condition or the type of care provided, these templates allow for uniformity and consistency in documenting patient discharge information.
Why is it Important ?
The discharge summary is a critical element in the continuum of care for several reasons:
Continuity of Care
The discharge summary aids in maintaining continuity of care. It provides subsequent healthcare providers with a complete overview of the patient’s condition during hospitalization, allowing them to make informed decisions about ongoing treatment and management.
Patient Safety
When well-composed and promptly provided, discharge summaries play a crucial role in patient safety. They outline post-discharge care instructions, including medication management, dietary advice, therapy recommendations, and follow-up appointment schedules. This guidance can help prevent unnecessary complications or readmissions.
Communication
The summary fosters effective communication between hospital-based physicians and primary care providers, specialists, patients, and caregivers. It ensures everyone involved in the patient’s care is informed of the patient’s health status and the next steps in their care.
Healthcare Quality Improvement
Discharge summaries can be used in population health management, research, and quality improvement initiatives. They offer valuable data about disease patterns, effectiveness of treatments, and patient outcomes.
Medicolegal Documentation
From a legal perspective, the discharge summary can provide important evidence about the care given to the patient during the hospital stay, which can be vital in case of legal concerns or insurance claims.
Coordination Between Care Settings
For patients moving to other care settings, such as rehabilitation centers, long-term care facilities, or home healthcare, the discharge summary facilitates the seamless transfer of crucial information.
What Should Be Included in a Hospital Discharge Summary?
Navigating the transition from hospital care to home or another healthcare facility involves a myriad of complex procedures. Central to this process is the Hospital Discharge Summary, a vital document that bridges the communication gap between hospital physicians and primary care providers.
It delivers a comprehensive overview of a patient’s hospital stay, serving as a valuable guide for post-hospital care. An effective discharge summary ensures continuity of care, reduces the risk of readmissions, and significantly improves patient safety and health outcomes. Let’s explore in-depth the elements that constitute a comprehensive Hospital Discharge Summary:
1. Patient Identification:
The discharge summary should begin with basic patient identification information. This typically includes the patient’s name, date of birth, hospital identification number, and gender.
2. Admission Date and Discharge Date:
These dates provide a timeline of the patient’s hospital stay. They are crucial for understanding the duration of treatment and hospitalization.
3. Reason for Admission:
This section details the primary reason or reasons that led to the patient’s hospitalization. It could be a specific medical condition, an accident, a surgical procedure, or a chronic illness exacerbation.
4. Diagnosis:
The discharge summary should include a clear and precise diagnosis or diagnoses established during the hospital stay. It is beneficial to provide both the initial diagnosis at the time of admission and the final diagnosis at the time of discharge.
5. Procedures and Treatments Provided:
This section should encompass all the significant medical or surgical procedures the patient underwent during their stay. It should also detail the treatments administered, including medication regimens, physical therapies, or any other interventions.
6. Hospital Course:
This part of the summary provides a narrative of the patient’s clinical progress during their hospital stay. It includes changes in the patient’s health status, response to treatments, any complications, and how these were managed.
7. Medication Reconciliation:
A thorough list of medications the patient is to continue post-discharge should be provided. This includes the drug name, dosage, frequency, route of administration, and purpose. It’s crucial to highlight any medication changes made during the hospital stay and provide reasons for these changes.
8. Follow-up Care Instructions:
Detailed guidance for post-discharge care is integral to the discharge summary. This may include wound care instructions, dietary restrictions, physical activity guidelines, and symptoms to watch for.
9. Pending Test Results and Future Investigations:
Sometimes, patients are discharged before all test results are available. In such cases, the summary should note these pending results and any additional tests or investigations that will be needed.
10. Appointments and Referrals:
The summary should specify any scheduled follow-up appointments and referrals to specialists or other healthcare services. It’s also helpful to include the contact information of these services.
11. Discharge Destination:
Finally, the summary should note where the patient is being discharged to, whether it’s their home, a rehabilitation center, a nursing home, or another healthcare facility.
How to Write a Discharge Summary
A well-drafted discharge summary is key to ensuring continuity of care once a patient leaves the hospital. This crucial document should provide a clear and concise overview of the patient’s hospital stay and a roadmap for their ongoing care. Here are the steps to create a comprehensive discharge summary:
Step 1: Begin with Patient Identification
Start the summary by documenting the patient’s essential details, including their name, date of birth, gender, and hospital identification number.
Step 2: Record the Dates of Admission and Discharge
Next, note down the dates when the patient was admitted and when they were discharged. These dates provide context for the duration of the hospital stay and treatment.
Step 3: Document the Reason for Admission
Provide a clear statement of the reason or reasons that led to the patient’s hospitalization.
Step 4: Include Diagnoses
Outline both the diagnosis at admission and the final diagnosis at the time of discharge. These diagnoses should be precise and fully reflective of the patient’s condition.
Step 5: Detail Procedures and Treatments
List all significant medical or surgical procedures the patient underwent during their stay. Additionally, include the treatments administered, such as medications, therapies, or other interventions.
Step 6: Describe the Hospital Course
Describe the patient’s clinical progress during their stay, including their response to treatments and any complications that arose, along with how these were managed.
Step 7: Complete Medication Reconciliation
Prepare a thorough list of medications the patient should continue post-discharge, including the name, dosage, frequency, route of administration, and purpose of each drug. Highlight any changes in medication and provide reasons for these changes.
Step 8: Provide Follow-up Care Instructions
Offer detailed instructions for post-discharge care, including any physical activity guidelines, dietary recommendations, and symptoms that should prompt the patient to seek medical attention.
Step 9: List Pending Test Results and Future Investigations
If the patient has been discharged before all test results are available, make a note of these pending results. Also, detail any additional tests or investigations needed.
Step 10: Schedule Appointments and Make Referrals
Include details of any scheduled follow-up appointments and referrals to specialists or other healthcare services. Provide contact information for these services to facilitate patient follow-up.
Step 11: Note the Discharge Destination
Finally, note where the patient is being discharged to, be it their home, a nursing home, or another healthcare facility.
Discharge Summary Example
Patient Identification:
- Name: John Doe
- Date of Birth: January 1, 1970
- Gender: Male
- Hospital ID: 123456
Admission Date: May 1, 2023
Discharge Date: May 14, 2023
Reason for Admission: John was admitted due to sudden onset severe chest pain, radiating to his left arm, and accompanying shortness of breath.
Diagnosis: On admission, John was suspected of having a myocardial infarction due to his presenting symptoms. This was subsequently confirmed through electrocardiogram (ECG) changes showing ST-segment elevation and laboratory results showing elevated cardiac troponin levels. The final diagnosis was ST-segment Elevation Myocardial Infarction (STEMI).
Procedures and Treatments Provided: John was immediately taken to the cardiac catheterization lab where he underwent an emergency percutaneous coronary intervention (PCI). A 90% stenosis of the left anterior descending artery (LAD) was identified and successfully managed with stent placement. He was then moved to the Cardiac Care Unit (CCU) for further management.
During his stay, John was initiated on dual antiplatelet therapy (aspirin and clopidogrel), a beta-blocker (metoprolol), a statin (atorvastatin), and an ACE inhibitor (lisinopril) for heart failure management. He also received comprehensive care including cardiac monitoring, pain management, nutritional support, and physical therapy.
Hospital Course: Post-procedure, John’s recovery was initially complicated by episodes of shortness of breath and a reduced ejection fraction on echocardiogram suggestive of heart failure. His medications were adjusted accordingly with the addition of an ACE inhibitor, and he was closely monitored for renal function and potassium levels. His condition gradually improved with these interventions. He also participated in hospital-based physical therapy to enhance his functional capacity before discharge.
Medication Reconciliation: Upon discharge, John is prescribed the following medications:
- Aspirin 81mg daily – For heart attack prevention
- Clopidogrel 75mg daily – For stent patency
- Metoprolol 50mg twice daily – For blood pressure control and heart protection
- Atorvastatin 40mg at bedtime – For cholesterol management
- Lisinopril 10mg daily – For heart failure management
Follow-up Care Instructions: John is advised to adhere to a low-sodium, low-cholesterol diet and engage in mild to moderate exercise as tolerated. He’s advised to seek immediate medical attention if he experiences chest pain, severe breathlessness, or any other concerning symptoms.
Pending Test Results and Future Investigations: No pending test results. He will need repeat lipid profile testing in 4 weeks to adjust atorvastatin dose as needed.
Appointments and Referrals: John has a follow-up appointment with his cardiologist in two weeks. He’s also referred to a dietitian for dietary advice and to a physical therapist for cardiac rehabilitation.
Discharge Destination: John is being discharged to his home, with his spouse present to assist in his care. Home healthcare services have been arranged to support his transition and recovery.
FAQs
Who receives a copy of the discharge summary?
Copies of the discharge summary are typically provided to the patient, the patient’s primary care physician, and any other healthcare providers involved in the patient’s ongoing care, such as specialists or therapists.
What should a patient do with their discharge summary?
Patients should review their discharge summary carefully to understand their medical condition, treatment received, and any post-discharge recommendations. It is important to keep a copy of the discharge summary for personal records and to share it with their primary care physician and other healthcare providers as needed.
How can a patient ensure effective post-discharge care based on the discharge summary?
To ensure effective post-discharge care, patients should follow the recommendations provided in the discharge summary. This may include taking prescribed medications, scheduling follow-up appointments, attending rehabilitation or therapy sessions, and making necessary lifestyle changes. It is also important to communicate any concerns or questions to the primary care physician or healthcare provider.
Can a patient request modifications or additional information in their discharge summary?
Yes, if a patient believes that certain information is missing or incorrect in their discharge summary, they can discuss their concerns with their primary care physician or the healthcare provider responsible for preparing the summary. It may be possible to make modifications or include additional information to ensure the accuracy and completeness of the document.
Is a discharge summary different from a medical report?
Yes, a discharge summary and a medical report serve different purposes. A discharge summary focuses on summarizing the details of a patient’s hospitalization, treatment, and recommendations for post-discharge care. On the other hand, a medical report is a broader document that may include information about a patient’s medical history, examination findings, diagnostic results, and treatment plans, often used for communication between healthcare providers or for legal purposes.
How long does it take to receive a discharge summary after being discharged from the hospital?
The time it takes to receive a discharge summary can vary depending on the hospital’s processes and the complexity of the case. In some cases, patients may receive the discharge summary on the day of discharge, while in other cases, it may take a few days to be prepared and sent to the patient and their primary care physician.
Can family members or caregivers obtain a copy of the patient’s discharge summary?
Yes, with the patient’s consent, family members or designated caregivers can usually obtain a copy of the patient’s discharge summary. The patient may need to sign a release of information form or provide verbal consent for the healthcare facility to share the summary with them.
Are discharge summaries standardized across all healthcare facilities?
While there are general guidelines for what should be included in a discharge summary, the format and specific content of the summary may vary between healthcare facilities. Some hospitals and healthcare systems may use standardized templates or electronic health record systems to ensure consistency, but there may still be variations in how information is presented.
What language is a discharge summary typically written in?
A discharge summary is usually written in the language that is commonly used in the healthcare facility or the patient’s country. In multilingual settings, efforts may be made to provide the discharge summary in the patient’s preferred language or provide translation services if needed.
Can a patient request a copy of their discharge summary at a later date?
Yes, patients can typically request a copy of their discharge summary at a later date if they need it for personal records or to share with other healthcare providers. They can contact the hospital or healthcare facility where they were treated and inquire about the process for obtaining a copy.
What should a patient do if they have questions or don’t understand something in their discharge summary?
If a patient has questions or doesn’t understand something in their discharge summary, they should contact their primary care physician or the healthcare provider responsible for their follow-up care. They can schedule an appointment or communicate through phone or secure messaging to discuss their concerns and seek clarification.
Are discharge summaries only provided for hospitalizations or are they also given after outpatient procedures?
Discharge summaries are typically associated with hospitalizations, where patients stay in the hospital for an extended period. However, for certain complex outpatient procedures or surgeries, a similar document may be provided that includes details of the procedure, post-procedure instructions, and recommendations for further care.
Can discharge summaries be accessed electronically or through online patient portals?
Yes, many healthcare facilities have implemented electronic health record systems and patient portals that allow patients to access their medical records, including discharge summaries, online. Patients can log into the patient portal, view, and download their discharge summary, and share it with other healthcare providers as needed.
Are discharge summaries confidential?
Yes, discharge summaries, like other medical records, are considered confidential and protected by patient privacy laws and regulations. Healthcare providers and facilities have a responsibility to ensure the security and confidentiality of patient information and should follow appropriate measures to safeguard the discharge summary and other medical records.
Can a patient request amendments to their discharge summary if they believe there are errors?
Yes, if a patient identifies errors or inaccuracies in their discharge summary, they can request amendments or corrections. They should contact the healthcare provider or hospital responsible for preparing the summary and provide the necessary information to support their request for revision. The healthcare provider will review the request and make appropriate changes if necessary.





































![Free Printable Roommate Agreement Templates [Word, PDF] 1 Roommate Agreement](https://www.typecalendar.com/wp-content/uploads/2023/06/Roommate-Agreement-150x150.jpg)
![Free Printable Credit Card Authorization Form Templates [PDF, Word, Excel] 2 Credit Card Authorization Form](https://www.typecalendar.com/wp-content/uploads/2023/06/Credit-Card-Authorization-Form-150x150.jpg)
![Free Printable Stock Ledger Templates [Excel,PDF, Word] 3 Stock Ledger](https://www.typecalendar.com/wp-content/uploads/2023/08/Stock-Ledger-150x150.jpg)
