Medical records are very important in the healthcare setting. Whether you’ve been working as a medical professional for many years or this is your first day on the job, you would want to know all the aspects of keeping medical records since they are necessary documents that could guide you when treating your patient. In this article, we will talk about examples of DAP (diagnostic assessment program) Note examples and how to use this type of note in hospital settings.
Table of Contents
What is a DAP note?

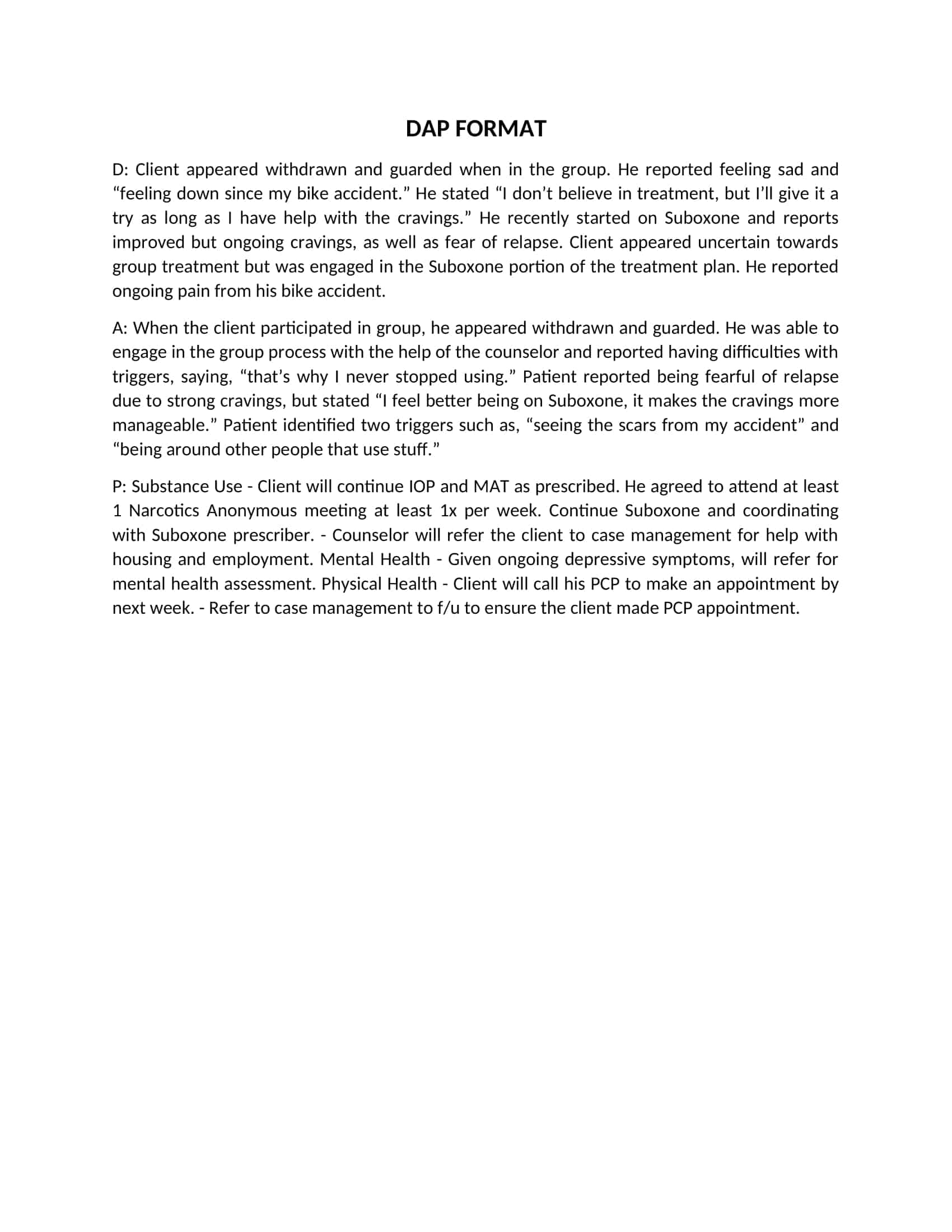
The Diagnostic Assessment Program (or DAP) is a medical record documentation standard that includes an assessment of the patient’s current condition, a plan for future treatment, and an action plan. These are known as “DAP Notes” or “DAP Notes Examples.” In hospitals, these notes are taken in addition to the ones the nurse takes at shift turnover before the physician sees the patient.
DAP Notes Templates
DAP notes are progress notes used by healthcare providers to document and analyze client data, goals, and treatment plans. DAP notes templates provide a standardized way to organize this information and facilitate communication among healthcare professionals.
These templates can be customized to fit the needs of different specialties and settings, including mental health, addiction treatment, and medical care. They can help providers stay organized, track progress, and provide effective care for their clients.
What goes in a DAP note?
Subjective observation
This section of your note should include what the patient tells you about their current symptoms, how they feel, and any other relevant information that may help you assess their condition.
Objective observation
The objective part of your note will include observations about how the patient looks and acts. For instance, if they appear to be nervous or anxious, this would be noted as an objective observation in your DAP note.
Assessment
Once you have completed your assessment using subjective and objective observations, it’s time to decide how best to proceed with treatment. Depending on the treatment plan, different options may be available for each diagnosis, such as medication or surgery. In this part of your DAP note, you need to decide which option is best for this particular case based on all the information gathered throughout the process of documenting progress through DAP notes.”
Plan
The plan section includes both short-term goals (for example, improving range of motion) and long-term goals (for example, returning to work). It should also include any instructions or advice for how long the patient should continue with their exercise program before coming back for another visit.
Tips for creating your DAP notes
The following are some tips for creating your DAP notes:
Define what the perfect note is
A good DAP note will include all relevant information about the client, including their demographics and symptoms. It should also include information about treatments and their progress. The best way to identify what makes for a great DAP note is to consult with your supervisor or other therapists who have experience taking DAP notes. Share your ideas with them and ask for theirs as well. They will be able to provide valuable insight into what makes for a winning DAP note example.
Keep things simple
It’s important to keep your notes concise and easy to read. You don’t want them to be so long that they become difficult for others to read or understand what they contain without having met with you directly first hand at least once before reading them either online or in hard copy form on paper via email attachments etc. For this reason, it’s essential that you keep things simple enough so that someone who hasn’t met with you before can figure out what they contain by just reading.
Use the tools that best suit your needs.
When taking these notes, you should consider using the tools that best suit your needs. There are many different options available when it comes to taking therapy session notes, and each one has its own advantages and disadvantages. For example, some programs may be more expensive than others or may require additional software programs such as Microsoft Word or Excel. Other programs may be free but have limited features and other limitations, such as not being able to print documents in full color or not being able to export data from the program into excel, which can hinder your ability to track information over time or analyze data properly.
Mistakes to avoid when writing DAP notes
DAP stands for “Discharge after Procedures.” These notes must be written by nurses who have been trained to use a standardized note format. They are used to document the patient’s condition at discharge from the hospital. They should summarize what happened during the hospitalization, including any procedures performed and medications given.
However, many nurses find it difficult to write DAP notes because they don’t know what to include or how to write them correctly. Here are some common mistakes that you should avoid when writing DAP notes:
Including too much information
Don’t forget that your notes are for your own use only. They’re not intended for patients or other healthcare professionals; therefore, there’s no need to include every piece of information listed in your chart. Only include information that you think will be useful when caring for this patient again in the future.
Using passive voice
In most cases, it’s best to use active voice when writing DAP notes because it makes sentences more direct and clear — not only for you but also for anyone else who might read them later on (e.g., another nurse or doctor). For example:
“The patient was given oral antibiotics.”
Don’t violate your patient’s privacy
This is a common mistake made by healthcare workers because they don’t realize that disclosing private information about a patient without his/her consent is illegal. It’s also unethical and bad for business.
Don’t include complaints about other staff members, whether from the patient, staff, or a doctor.
These complaints might not be true and could damage colleagues’ relationships. This can easily happen when multiple people treat a patient at once, such as during an admission. If there are concerns about another member of the team or their performance, address them directly with them instead of including them in your notes or talking about them openly with other staff members.
Don’t ever include any disparaging or derogatory statements about your patient.
There is no reason for you to write anything negative about your patient in their DAP notes unless it relates specifically to their care or treatment plan (e.g., “patient refused all medications”). If you have any negative feelings toward your patient, keep them to yourself and do not write them down anywhere.
FAQs
What are DAP notes?
DAP notes document a client’s progress in therapy using three components – the Date the session took place, an Assessment of the client’s current presentation, and the clinician’s Plan for future sessions or treatment.
What should be included in the Assessment?
The assessment should summarize the main themes discussed during the session, the client’s mood and affect, any critical incidents, mental status observations, risk assessments, and progress on treatment goals. Keep it concise yet detailed.
How do you write an effective Plan?
The plan section outlines follow-up items, agreed next steps, referrals, and upcoming session goals. Be specific about assigning homework or tasks. Avoid vague statements.
What makes DAP notes clinically useful?
Good DAP notes are succinct yet capture critical details about the client’s mental health status and progress to inform diagnosis and continuity of care. Use client quotes to illustrate thinking. Avoid jargon. Written objectively in third-person.
How do you write them quickly?
Being organized, having a template, using abbreviations/shortcuts, employing apps and voice transcription can all help streamline note-taking. But don’t sacrifice quality for speed. Notes should be comprehensive and clear.































![Free Printable Roommate Agreement Templates [Word, PDF] 1 Roommate Agreement](https://www.typecalendar.com/wp-content/uploads/2023/06/Roommate-Agreement-150x150.jpg)
![Free Printable Credit Card Authorization Form Templates [PDF, Word, Excel] 2 Credit Card Authorization Form](https://www.typecalendar.com/wp-content/uploads/2023/06/Credit-Card-Authorization-Form-150x150.jpg)
![Free Printable Cornell Notes Templates [PDF, Word] 3 Cornell Notes](https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-150x150.jpg 150w, https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-120x120.jpg 120w, https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-1200x1200.jpg 1200w)
