As a nursing professional, you often find yourself at the forefront of critical medical scenarios. In the performance of your role, you are required to document each patient interaction meticulously.
These records carry immense significance as you are primarily the individual responsible for dispensing medications to patients within the healthcare facility. It is therefore vital to master the art of crafting concise and efficient nursing note samples that can be referenced as necessary.
Table of Contents
What is a Nursing Progress Notes Template?

A Nursing Progress Notes Template is a standardized tool used by nurses or healthcare professionals to systematically record the details of a patient’s health condition and the treatment they are receiving. This kind of documentation helps ensure consistent, comprehensive, and efficient communication between all members of a healthcare team.
Nursing Notes Templates
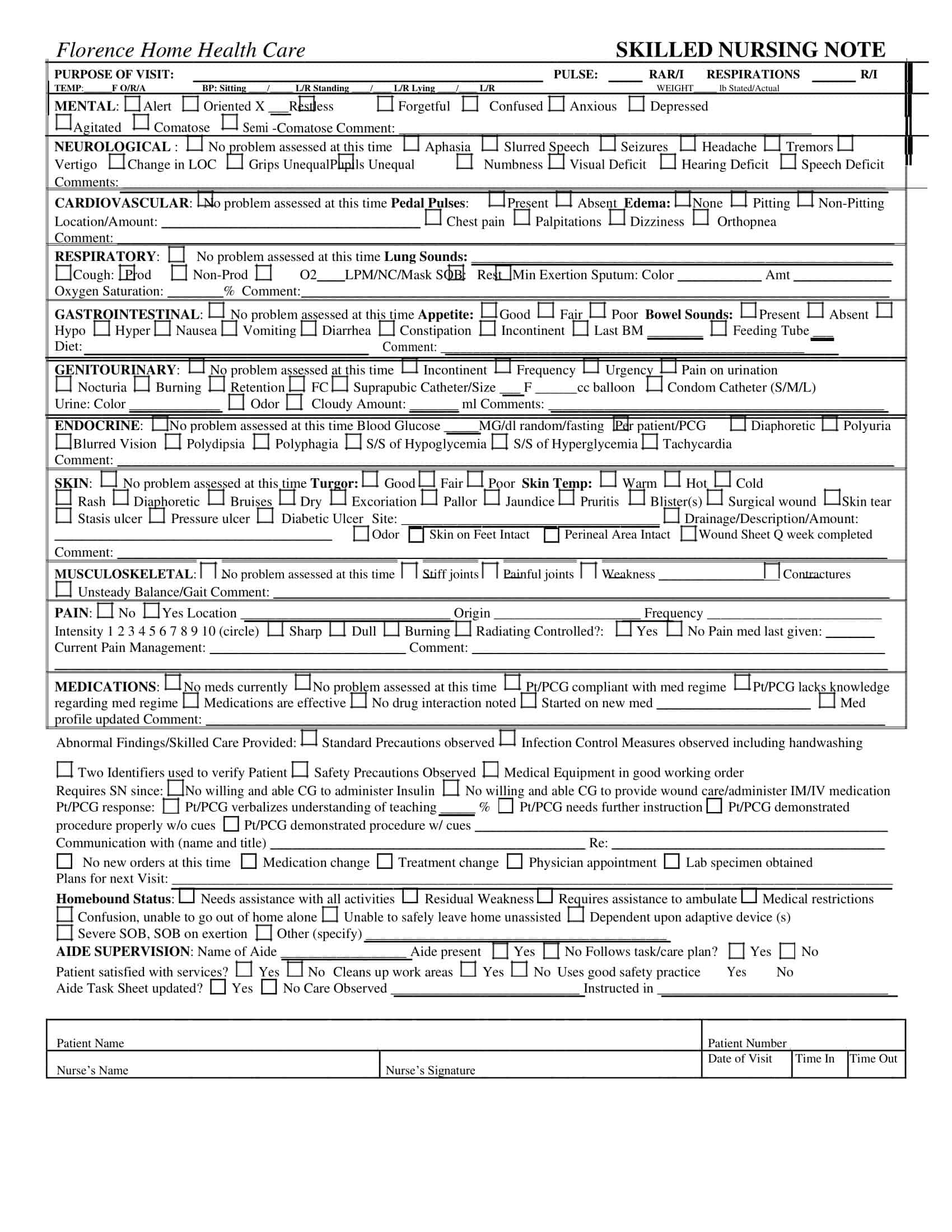
Nursing Notes Templates are organized structures used by nurses to document essential patient information. These templates serve as a critical part of patient health records, ensuring that crucial information is accurately and consistently recorded.
Typically, these templates include sections for patient identification, date and time, and an area to record patient observations, treatment administered, and responses to treatment. Some templates might also include areas to note changes in the patient’s condition, plans for continued care, and any patient or family education provided.
Nursing Notes Templates are designed to encourage thorough, consistent documentation. This consistent documentation is a critical factor in providing seamless healthcare services, facilitating communication among healthcare providers, and ensuring the continuity of patient care.
Understanding the Significance of Thorough Nursing Note Writing
The practice of writing nursing notes, also known as documentation or charting, is an essential part of a nurse’s role and carries significant benefits in the realm of healthcare. Here are some of the primary advantages:
- It helps enhance communication among healthcare professionals, ensuring everyone involved in a patient’s care is up-to-date with their condition and treatment plan.
- It helps in coordinating care across different shifts and specialties, making the transition of care seamless and efficient.
- It helps provide legal protection, serving as an objective and thorough record that can be referred to in the event of legal issues or malpractice claims.
- It helps in tracking and evaluating a patient’s progress over time, facilitating the identification of patterns and the understanding of treatment effectiveness.
- It helps in quality improvement and auditing processes, enabling healthcare facilities to identify areas for improvement and comply with accreditation standards.
- It helps ensure appropriate reimbursement from insurance providers by documenting the necessity and delivery of specific treatments or procedures.
- It helps in education and research, serving as a rich resource for learning and data collection in clinical studies.
- It helps promote reflective practice among nurses, encouraging critical thinking, self-evaluation, and continuous improvement in patient care.
Elements to include in a nursing note
Nursing notes are crucial tools for communicating patient information, tracking patient progress, and guiding care decisions. To be effective, these notes must be accurate, comprehensive, and consistent. Below are key elements that should be included in a nursing note:
- Patient Identification Information: Start with the patient’s basic information, such as their full name, date of birth, and unique patient ID number.
- Date and Time: All entries should be accurately timestamped. This helps in tracking the progression of the patient’s condition and ensures the chronology of care is clear.
- Subjective Data: This refers to information provided by the patient, including their symptoms, feelings, concerns, and personal observations. Remember to quote the patient’s own words when possible to avoid misinterpretation.
- Objective Data: These are measurable and observable facts about the patient’s condition, such as vital signs (blood pressure, pulse, temperature, respiratory rate), physical examination findings, lab results, and other test results.
- Assessment: This is the nurse’s professional judgement or interpretation based on the combination of subjective and objective data. It should address any changes in the patient’s condition and how they are responding to treatment. If applicable, relate this data to a specific diagnosis or condition.
- Plan/Intervention: This outlines the actions taken in response to the assessment. It might include administering medications, performing procedures, patient education, referrals, or preparations for diagnostic tests or surgeries.
- Evaluation: Document the patient’s response to the interventions or treatments. This will help determine whether the plan needs to be continued, revised, or discontinued.
- Future Care Plan: Provide an overview of future care plans, changes in treatment, or goals for the patient.
- Signature: Finally, sign the nursing note to verify that all the information provided is accurate. This should include your full name, title, and credentials.
Types of Nursing Notes
Nursing notes, also known as nursing documentation, can take various forms, each designed to capture a specific type of information about a patient’s status, care, and progress. Here are several types of nursing notes that are commonly used in healthcare settings:
Narrative Nursing Notes
These are traditional, free-text notes that provide a comprehensive story of a patient’s care. The nurse writes a continuous account of the patient’s status, care, and response in chronological order. While this format allows for detailed documentation, it can be time-consuming and often leads to redundant information.
SOAP Notes
SOAP stands for Subjective, Objective, Assessment, and Plan. This structured format is often used for problem-oriented documentation.
- Subjective: The patient’s feelings, symptoms, concerns, and history from the patient’s perspective.
- Objective: Observable and measurable information such as vital signs, physical examination findings, and lab results.
- Assessment: The nurse’s professional interpretation of the subjective and objective data.
- Plan: The planned interventions, which could include treatments, patient education, or further testing.
Focus Charting (DAR)
This method uses Data, Action, and Response to structure nursing notes.
- Data: Information that supports the focus or identified issue, which can be a patient concern, change, or strength.
- Action: Interventions performed by the nurse.
- Response: The patient’s response to the intervention.
PIE Notes
PIE stands for Problem, Intervention, and Evaluation.
- Problem: Identified patient problem or nursing diagnosis.
- Intervention: Actions taken to address the problem.
- Evaluation: Assessment of the effectiveness of the interventions.
Charting by Exception (CBE)
This system involves only documenting findings that are outside the normal range or deviations from the established care plan. It is time-efficient but relies on comprehensive policies and defined standards to identify what ‘normal’ and ‘abnormal’ are.
Electronic Health Records (EHR)
These are digital versions of patient charts, where nursing notes are recorded using pre-set templates on a computer system. They improve readability, reduce redundancy, and allow for efficient sharing of information.
Critical Pathways
These are standardized care plans for a specific diagnosis, procedure, or health condition. They outline the expected progress and outcomes, and any deviation from the pathway is documented.
Each type of nursing note has its strengths and weaknesses, and the choice often depends on the situation, the healthcare setting, and the specific needs of the patient. Regardless of the format used, it’s essential that nursing notes are accurate, concise, and complete to ensure the highest level of patient care.
How To Write a Nursing Note
Writing nursing notes is a crucial skill for nurses and other healthcare professionals. It provides a record of the care given to patients and serves as a means of communication among healthcare team members. Here is a detailed step-by-step guide on how to write an effective nursing note:
Prepare
Before writing the note, make sure you have all the necessary information at hand. This may include recent lab results, the patient’s current status, the care provided, and the patient’s response to the treatment. Gather your thoughts and organize them.
Patient Identification
Start your note with the patient’s identifying information. This typically includes the patient’s name, date of birth, and unique ID number. This should be in line with your institution’s guidelines for patient identification.
Date and Time
Record the date and time of each entry. This ensures a clear chronology and helps other healthcare professionals understand the timeline of the patient’s care.
Subjective Data
Record any information the patient (or their family) provides about their symptoms, feelings, concerns, or history. Use direct quotes when possible to avoid misinterpretation. For instance, “Patient reports feeling ‘very tired’ today.”
Objective Data
Document factual, observable, and measurable data. This includes vital signs, physical exam findings, lab results, medication administration, and other observable indicators. Be as specific and accurate as possible.
Assessment
Provide your professional interpretation of the subjective and objective data. Describe the patient’s current health status and progress. Connect this information to the patient’s diagnosis or condition if applicable.
Plan/Intervention
Describe the actions taken or to be taken in response to your assessment. This could be the administration of medication, a change in treatment, a referral to a specialist, patient education, or preparations for tests or procedures.
Evaluation
Document the patient’s response to the interventions or treatments. This information will help guide future care decisions.
Future Care Plan
Write down the proposed plan for future care. This could include changes to the treatment plan, upcoming procedures, or goals for the patient.
Review and Signature
Review your note to ensure it’s accurate, clear, and complete. Once you’re sure it’s correct, sign the note with your full name, title, and credentials.
Nursing Note Examples
Here are examples of a nursing note written in the SOAPIE and DAR formats:
SOAPIE Example
| Section | Details |
| Subjective | Patient is a 65-year-old male presenting with acute onset of severe, sharp chest pain radiating to the left arm, and associated shortness of breath. Patient rates pain as 8/10 in severity. |
| Objective | Parameter Observation Vital Signs Vital Sign Results Blood Pressure 145/90 mmHg Pulse 100 bpm Respiratory Rate 22 breaths/min Temperature 98.6 F SpO2 92% Physical Examination Patient appears anxious with pallor and diaphoresis. Chest examination reveals decreased breath sounds in the left lower zone. Heart sounds are regular but rapid. Investigations Investigation Results ECG Pending Blood Tests (Troponin, CBC, Electrolytes) Pending |
| Assessment | Patient with symptoms and signs suggestive of acute coronary syndrome, possibly an acute myocardial infarction. Further investigations are required to confirm the diagnosis. |
| Plan | Notify the medical team immediately. Administer 300mg of chewable aspirin, pending doctor’s approval. Administer oxygen therapy to keep SpO2 above 94%. Prepare for possible ECG and further cardiac investigations. Administer nitroglycerin as per protocol, if ordered by the doctor. Prepare for possible transfer to the intensive care unit or cardiac care unit. Continuously monitor patient’s vital signs, oxygen saturation, and symptoms. Document changes and notify the medical team as required. Patient education: Explain the situation to the patient and his family, answer any questions, provide reassurance as appropriate. |
DAR (Data, Action, Response) Example
| Section | Details |
| Data | Parameter Observation Patient Description Patient is an 80-year-old female with a history of dementia, recently admitted for a urinary tract infection. Vital Signs Vital Sign Results Blood Pressure 130/70 mmHg Pulse 78 bpm Respiratory Rate 16 breaths/min Temperature 99.2 F SpO2 96% Observations Patient appears to be uncomfortable and keeps touching the genital area. Increased agitation noted compared to the usual state. |
| Action | Assessed the patient for any sign of distress. Checked the patient’s catheter for any signs of blockage or improper positioning. Collected a urine sample for urinalysis to assess for potential urinary tract infection. Notified the healthcare provider about the patient’s change in behavior and the suspicion of a urinary tract infection. |
| Response | Upon repositioning the catheter, the patient appeared to be less agitated. Patient’s vital signs remained stable after the action. The healthcare provider ordered a urinalysis and urine culture, results are pending. The healthcare provider also ordered a pain assessment to be completed during the next few interactions with the patient to ensure appropriate pain management. |
Tips for Writing Effective Nurse Notes
Writing effective nursing notes ensures the delivery of safe, consistent, and legal healthcare. Here are detailed guidelines and examples to assist in enhancing your nursing documentation skills:
- Be Accurate and Specific: Your descriptions should be detailed and precise. Instead of writing “Patient is in pain,” provide specifics such as “Patient reports sharp, stabbing pain in the lower abdomen rated 8 on a scale of 1 to 10.”
- Be Timely: Record notes immediately after an event or patient interaction. This increases accuracy and reduces memory-related errors. For example, after administering medication, immediately document the type of medication, dosage, route, and the patient’s immediate response.
- Maintain Professionalism: Use clinical and non-derogatory language. Instead of writing “Patient was difficult during the shift,” write “Patient displayed signs of agitation and resisted oral medication administration.”
- Use Approved Abbreviations: Use only commonly accepted abbreviations to prevent misinterpretation. For instance, use “b.i.d” for twice a day, but avoid uncommon or facility-specific abbreviations without explaining them.
- Be Concise: Make your notes straightforward and to the point. Instead of a lengthy narrative, write “Patient ambulated 50 feet down the hallway with one rest stop, using a walker, and assistance from one staff for safety.”
- Stick to the Facts: Base your notes on your professional observations or measured data. Rather than writing “Patient might have an infection,” write “Patient has a temperature of 101.6°F, increased heart rate, and redness and swelling at surgical site.”
- Document Chronologically: Record your notes in a timeline to ensure clarity of the sequence of events. For instance, “07:00 – Patient complained of shortness of breath; 07:05 – Administered 2L of oxygen via nasal cannula; 07:20 – Patient’s breathing appears more comfortable.”
- Patient’s Words: Use direct quotes when the patient or family gives information. If a patient says, “I feel like I’m drowning,” record it as a quote in your notes.
- Sign and Date Your Entries: Each entry must be signed with your full name, credentials, and the current date and time, such as “6/17/2023, 09:30 – J. Doe, RN.”
- Maintain Confidentiality: Only include relevant patient information. Instead of writing “Patient, a famous musician, admitted for alcohol withdrawal,” write “Patient admitted for alcohol withdrawal.”
- Write Legibly: If handwriting, ensure your notes are easy to read. Illegible writing can cause misinterpretation and errors in the patient’s care.
- Use a Consistent Format: Adopt a standard note-taking format, like SOAP or DAR. This helps streamline your documentation and ensures all necessary aspects of care are covered.
- Proofread: Review your notes to check for errors or unclear statements. A note stating “Patient fell, no injury,” could be better written as “Patient had an unassisted fall, no visible injury noted, vital signs stable.”
- Record Refusals: Document any instances of patient refusal. For example, “Patient refused evening medication, stating it makes him too drowsy.”
FAQs
Can a nursing note be corrected?
Yes, a nursing note can be corrected if an error is found. However, it’s important to follow proper procedures to maintain the document’s integrity. Usually, this involves drawing a single line through the error, initialing, and dating the correction, then writing the correct information. Never erase or use correction fluid on a nursing note.
Who can access nursing notes?
In general, the patient, the healthcare team involved in the patient’s care, and authorized personnel within the healthcare facility can access nursing notes. The patient can also grant permission for others to access their medical records, including nursing notes. In certain cases, legal professionals may also access nursing notes, such as in a malpractice lawsuit.
What is the difference between a nursing note and a progress note?
Both are part of a patient’s medical record and document the patient’s status and care. However, nursing notes are written by nurses and often focus on daily care, patient behavior, and responses to treatment. Progress notes are typically written by physicians or other healthcare providers and focus more on the diagnosis, treatment plan, and the patient’s progress towards their health goals.
What should not be included in a nursing note?
Nursing notes should not include any judgmental language, personal opinions, irrelevant information, or abbreviations that are not universally accepted. Confidential information unrelated to the patient’s treatment should also be excluded. Additionally, speculative comments or diagnosis, which are not within a nurse’s scope of practice, should not be included.
Can a nursing note be used in court?
Yes, nursing notes can be used as evidence in court. They form part of the patient’s medical record and can be critical in cases such as malpractice lawsuits or personal injury claims. Hence, it is important for the notes to be accurate, factual, and complete.
How long should nursing notes be kept?
The length of time nursing notes should be kept can vary by jurisdiction and hospital policy. Generally, they are kept for several years after the patient’s last contact with the healthcare provider. For pediatric patients, the records are often kept until the patient reaches adulthood plus a certain number of years.
Is electronic nursing documentation different from traditional paper documentation?
The content and purpose of electronic and paper documentation are the same – to record the patient’s status, care, and progress. However, electronic documentation often has the advantage of being easier to read, access, and share. It can also include prompts for necessary information, reducing the chance of missing data.
What is charting by exception in nursing notes?
Charting by exception is a style of documentation where only significant or abnormal findings are noted. This method operates under the assumption that all standards of practice are carried out and met unless otherwise documented. It can save time but may risk missing important information if not done carefully.





























![Free Printable Roommate Agreement Templates [Word, PDF] 1 Roommate Agreement](https://www.typecalendar.com/wp-content/uploads/2023/06/Roommate-Agreement-150x150.jpg)
![Free Printable Credit Card Authorization Form Templates [PDF, Word, Excel] 2 Credit Card Authorization Form](https://www.typecalendar.com/wp-content/uploads/2023/06/Credit-Card-Authorization-Form-150x150.jpg)
![Free Printable Stock Ledger Templates [Excel,PDF, Word] 3 Stock Ledger](https://www.typecalendar.com/wp-content/uploads/2023/08/Stock-Ledger-150x150.jpg)
