SOAP notes are an essential tool for healthcare professionals, providing a structured format for documenting patient treatment and progress. Used in hospitals and clinics worldwide, SOAP notes are a key component of medical records and are used to update patient information, communicate with other healthcare providers, and provide proof of regular and effective treatment. In this article, we will explore the importance of SOAP notes, provide examples of SOAP note templates, and offer tips and strategies for creating effective SOAP notes.
Table of Contents
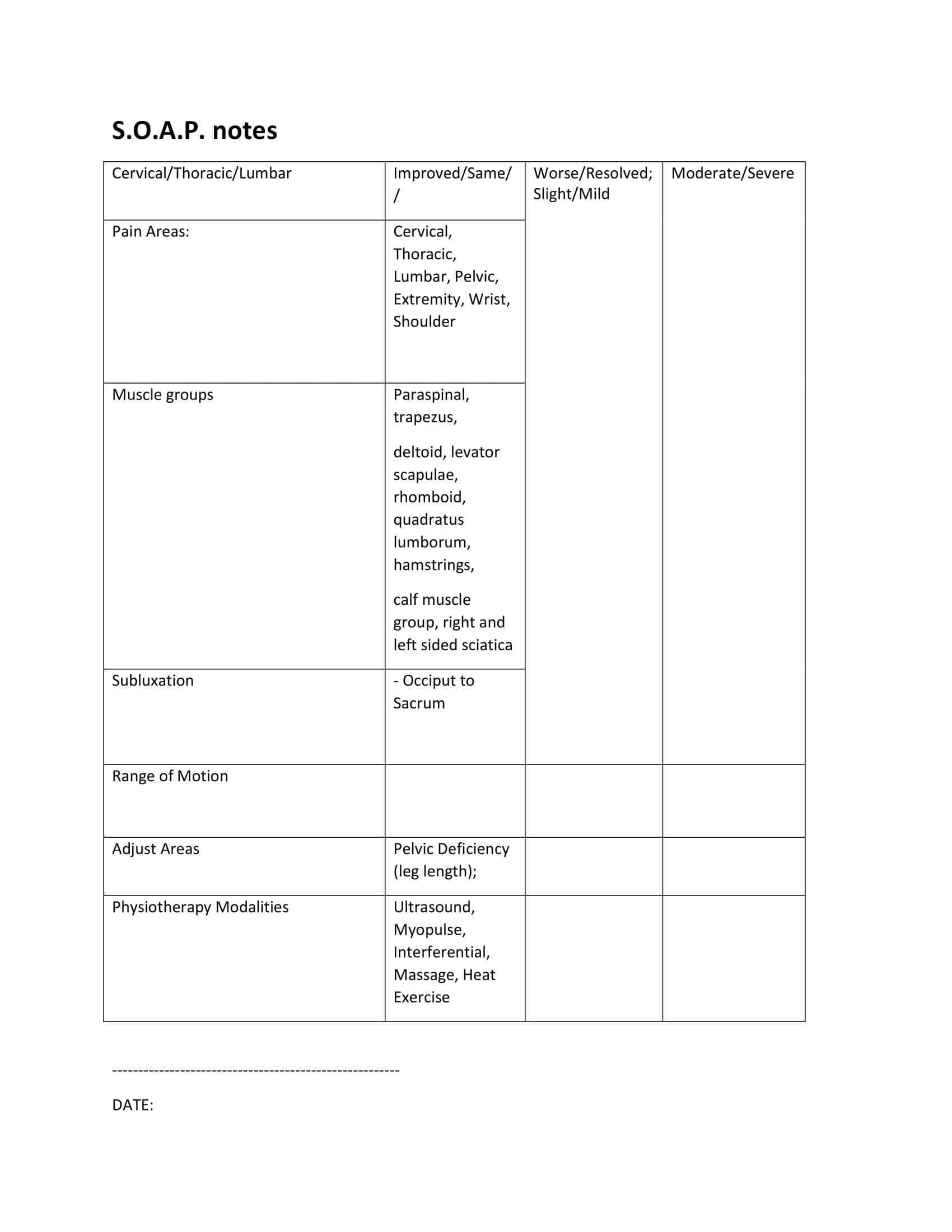
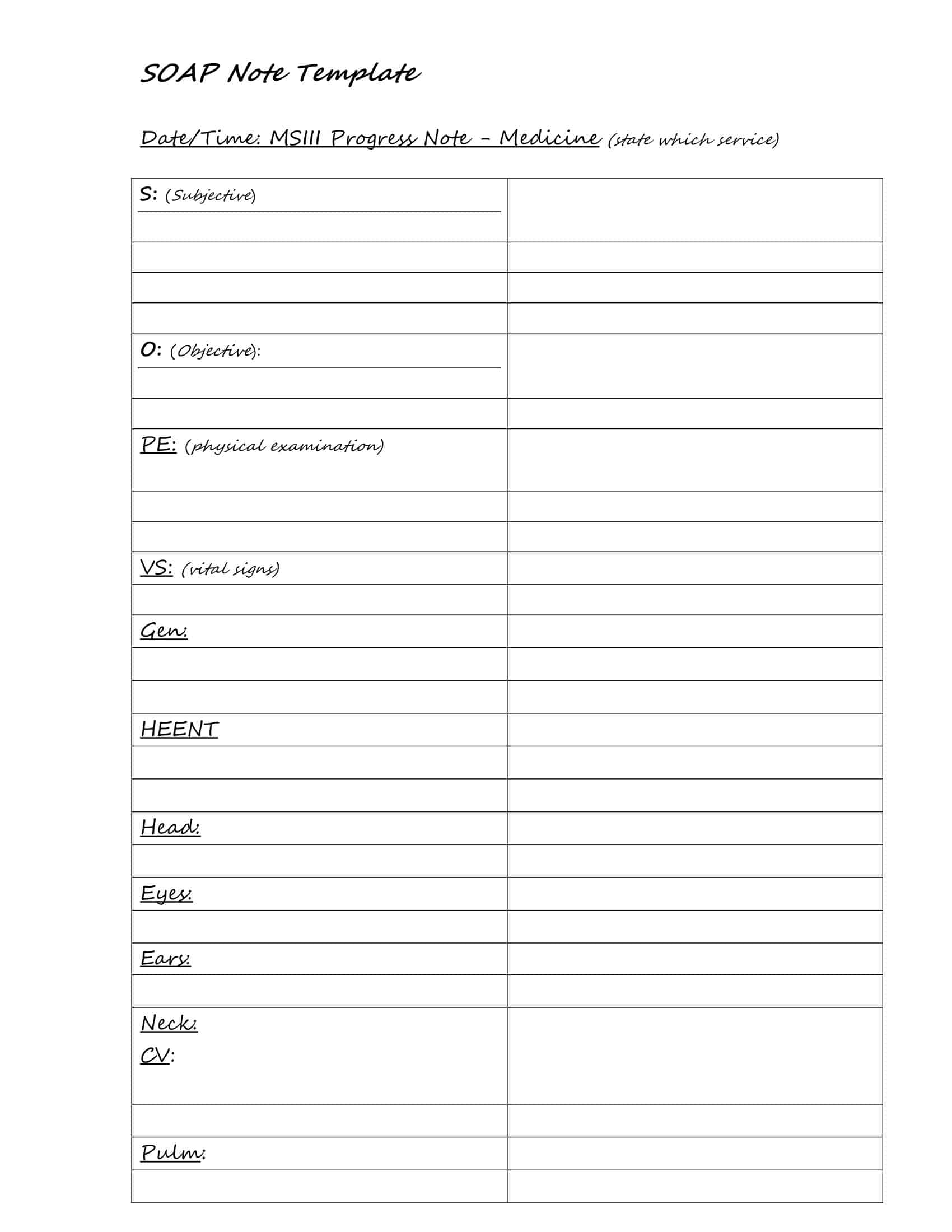
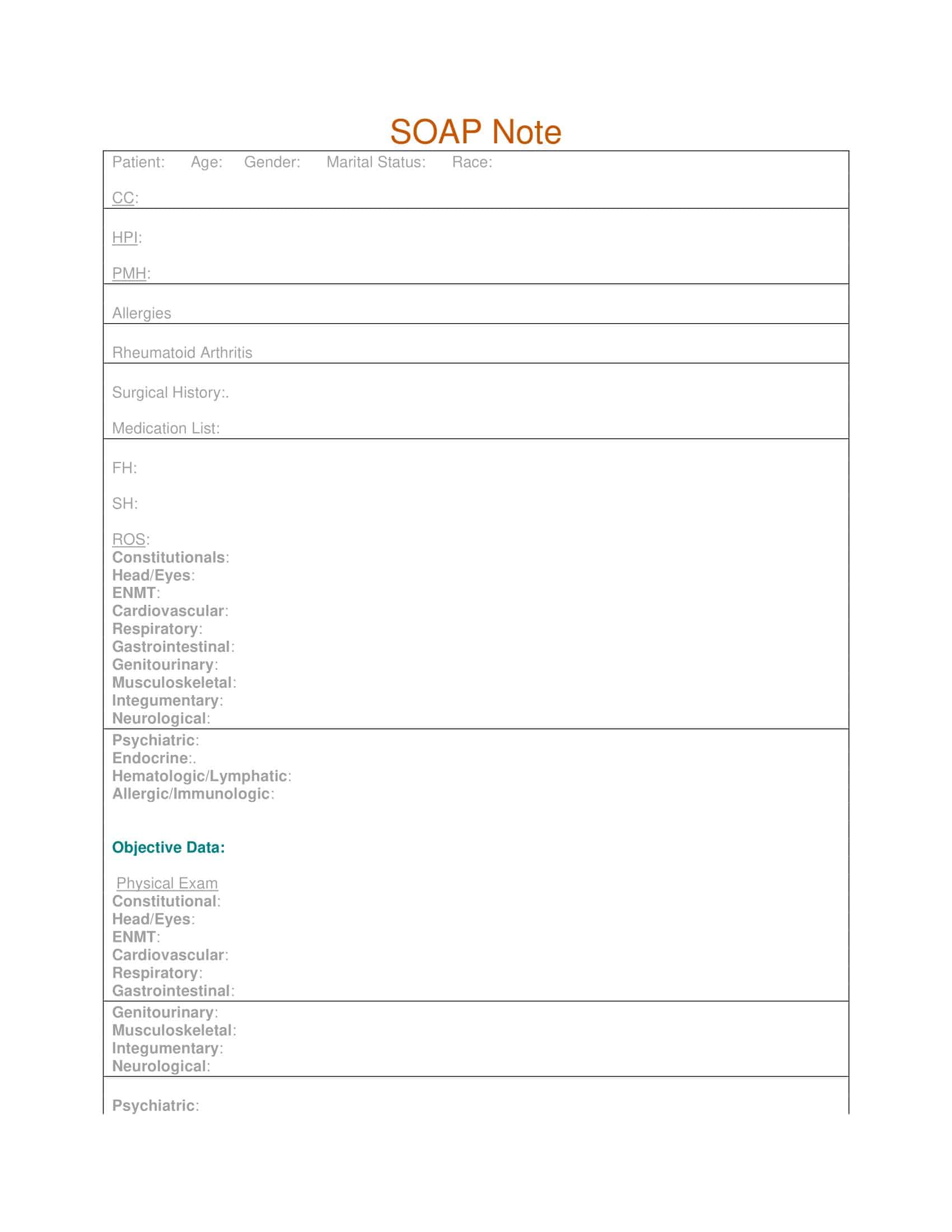
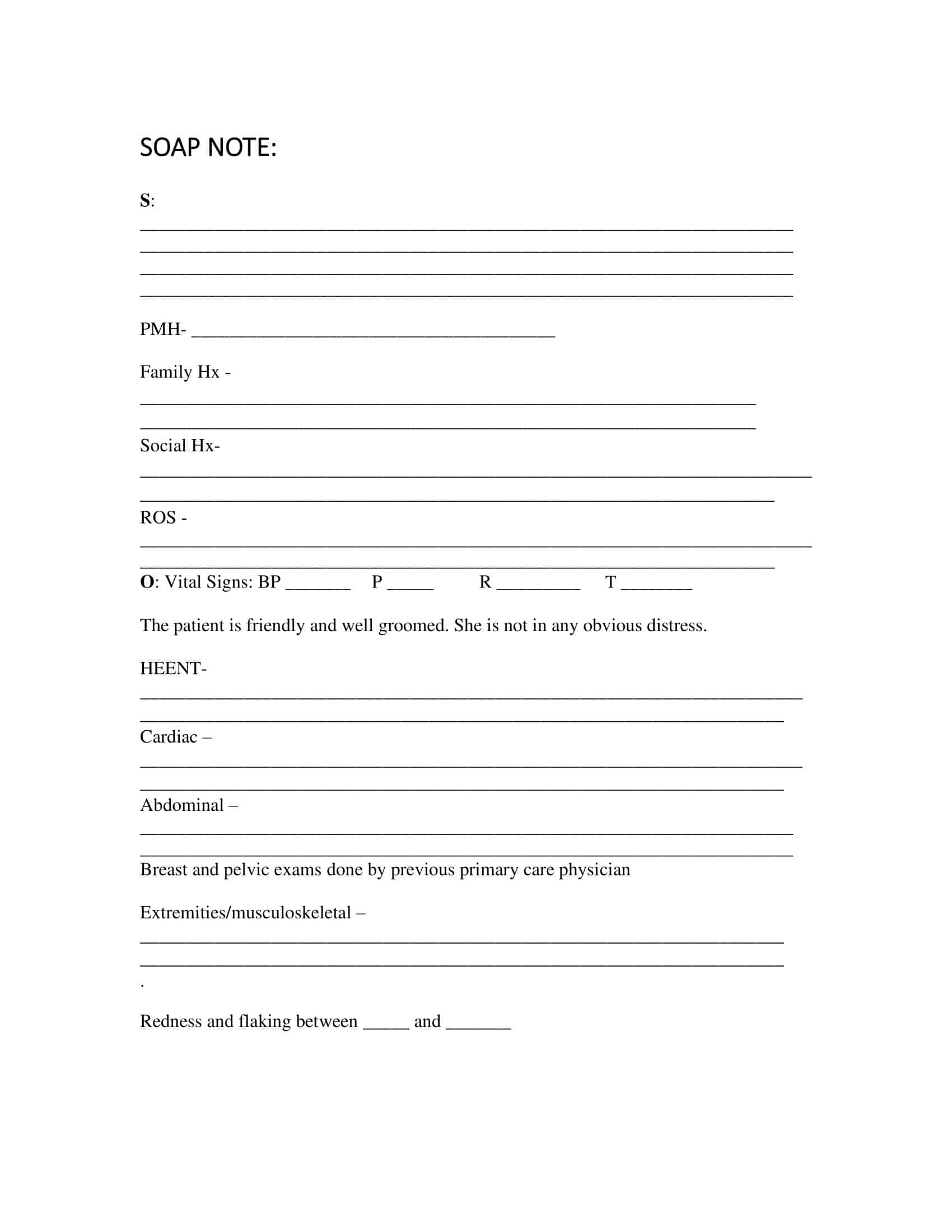
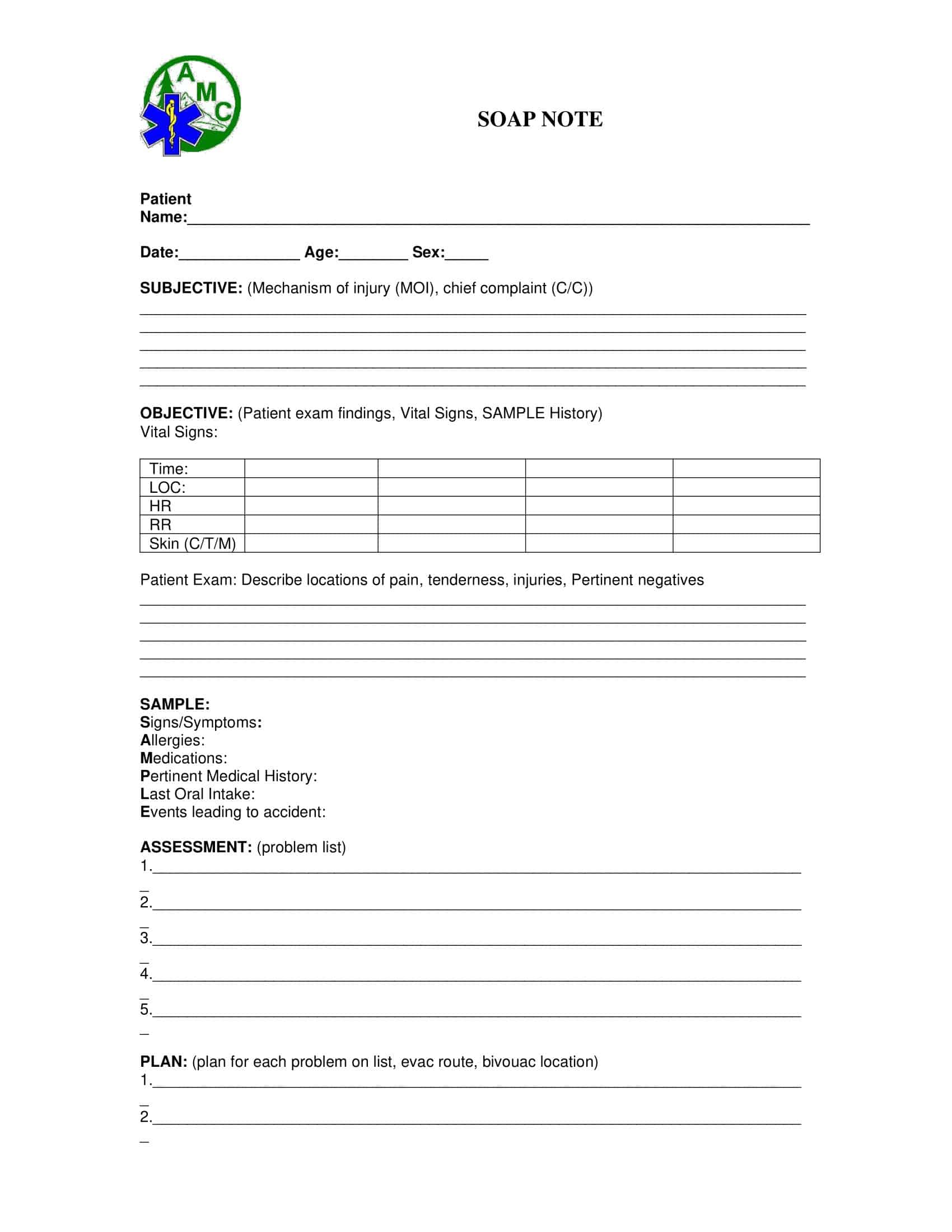
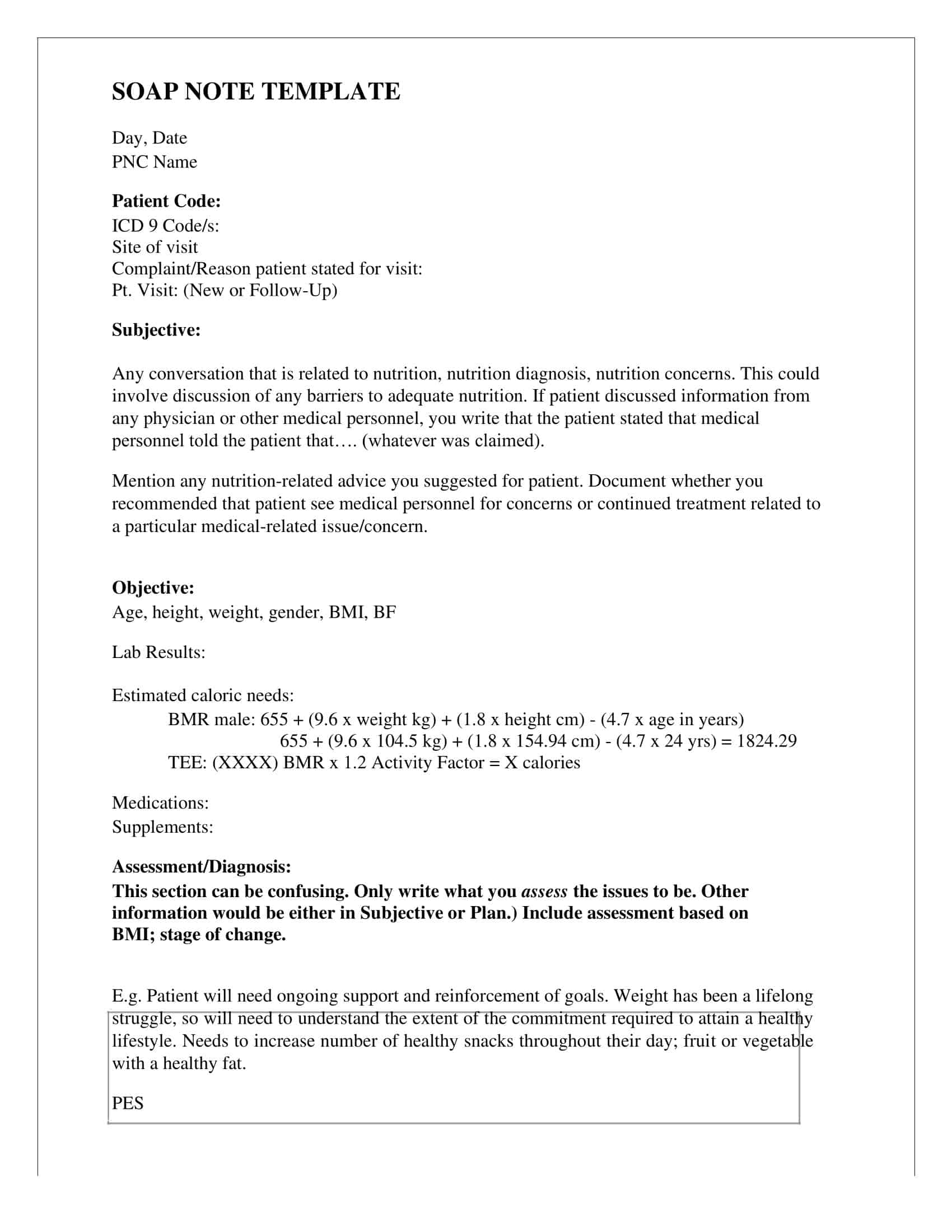
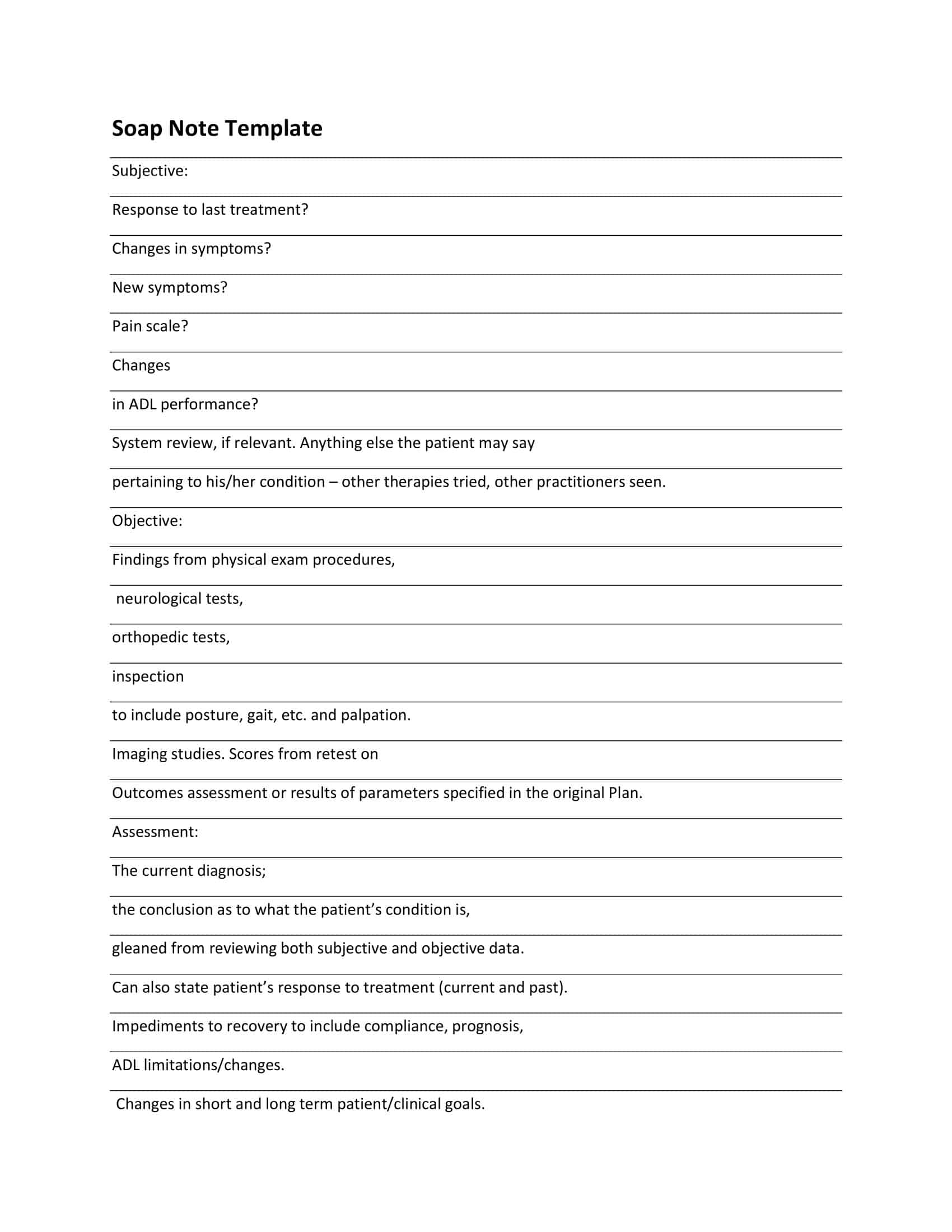
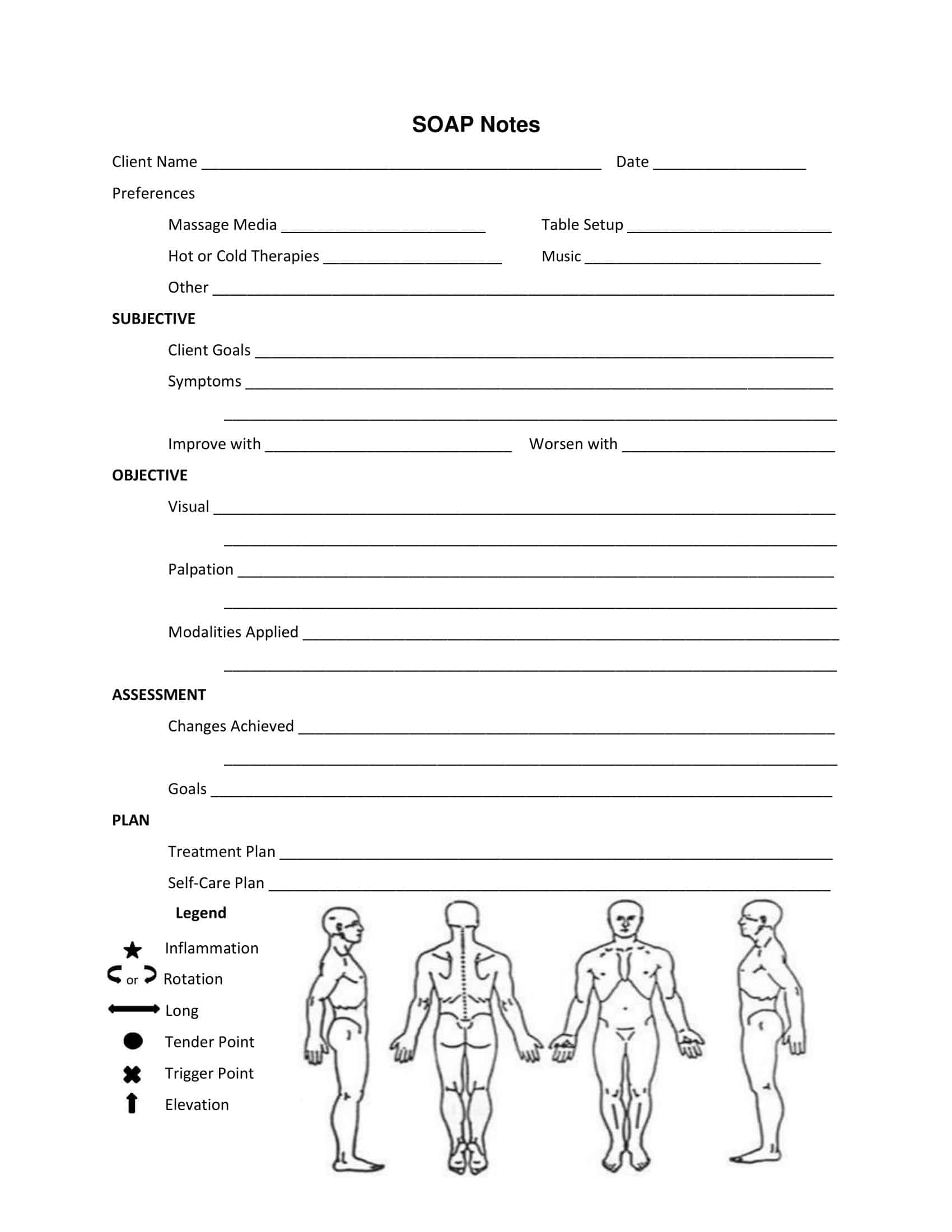
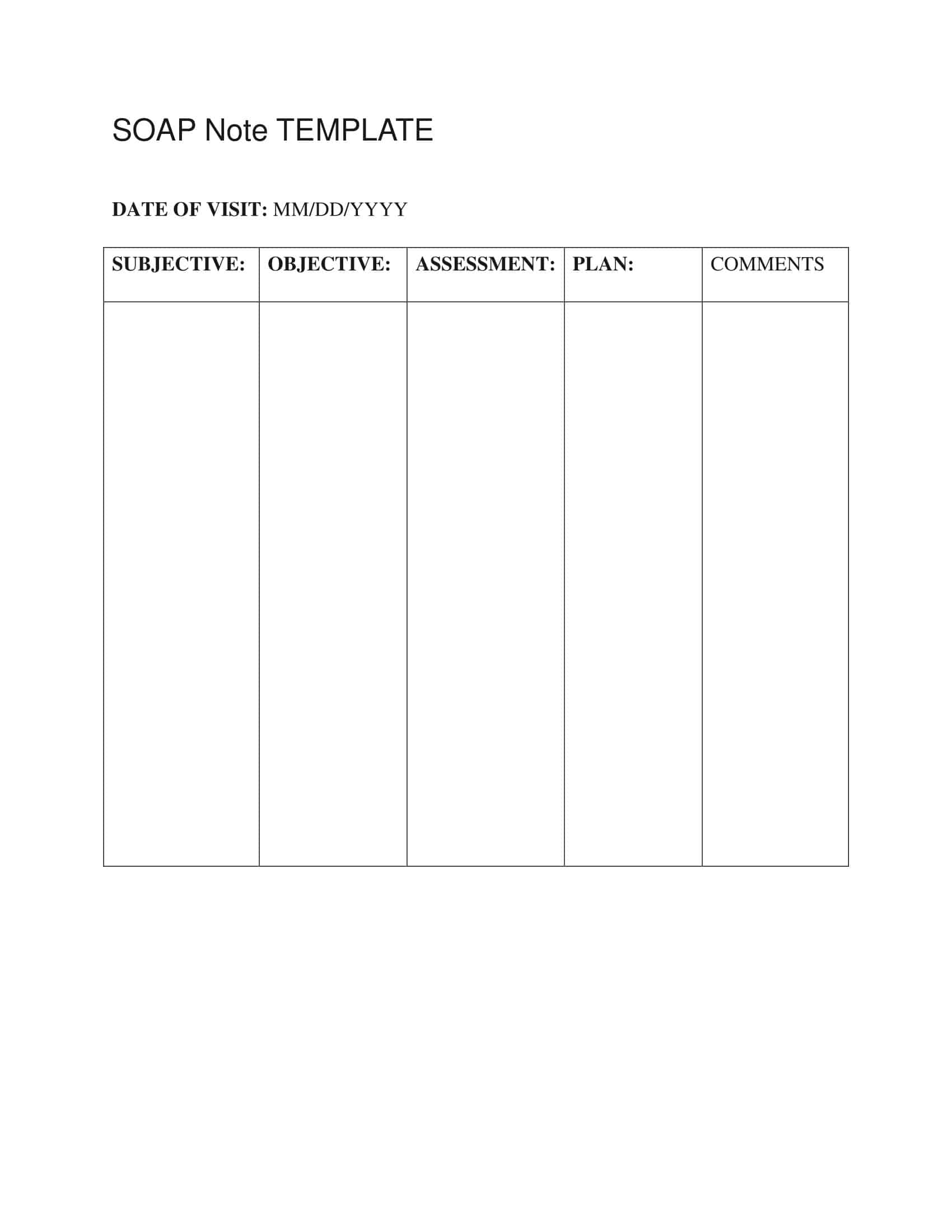
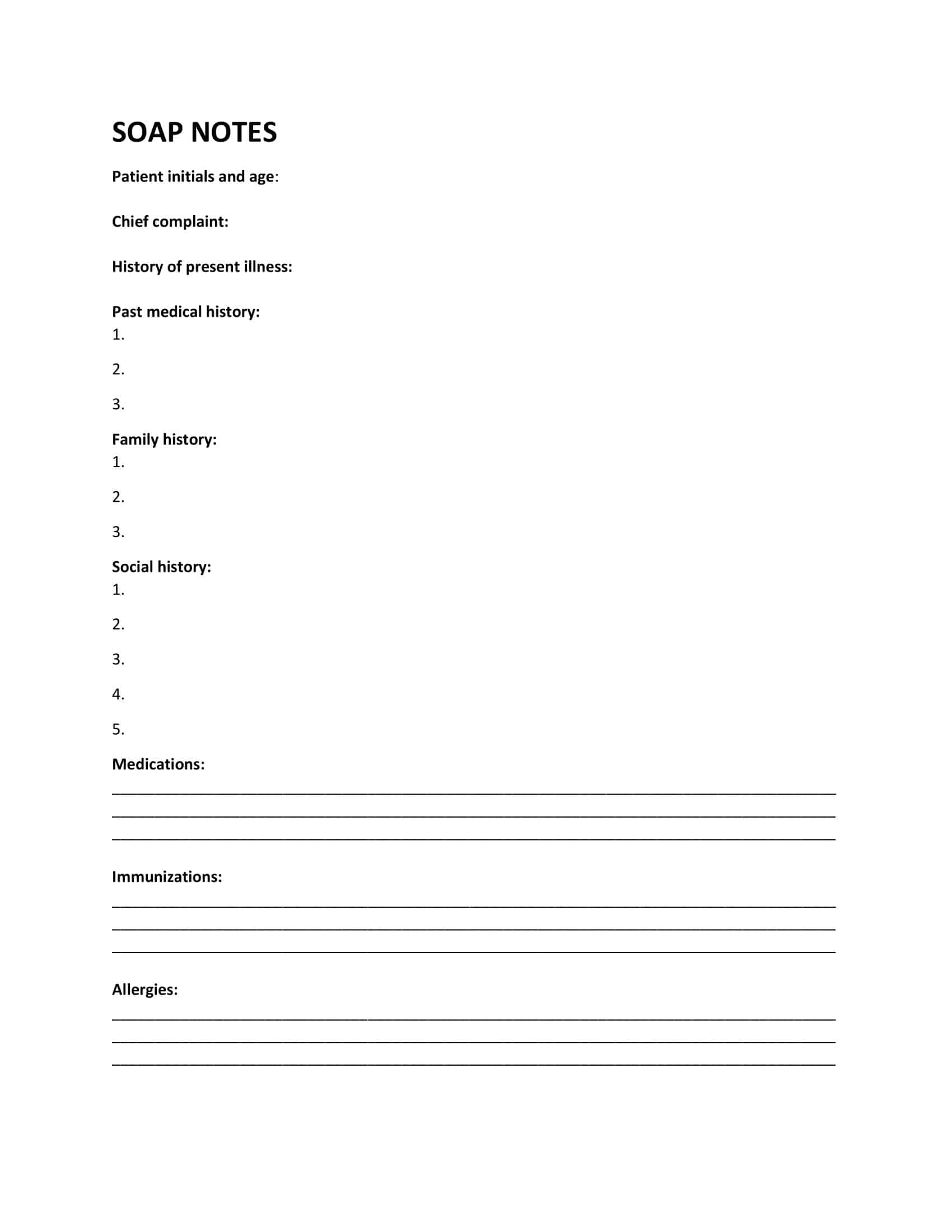
SOAP Note Templates
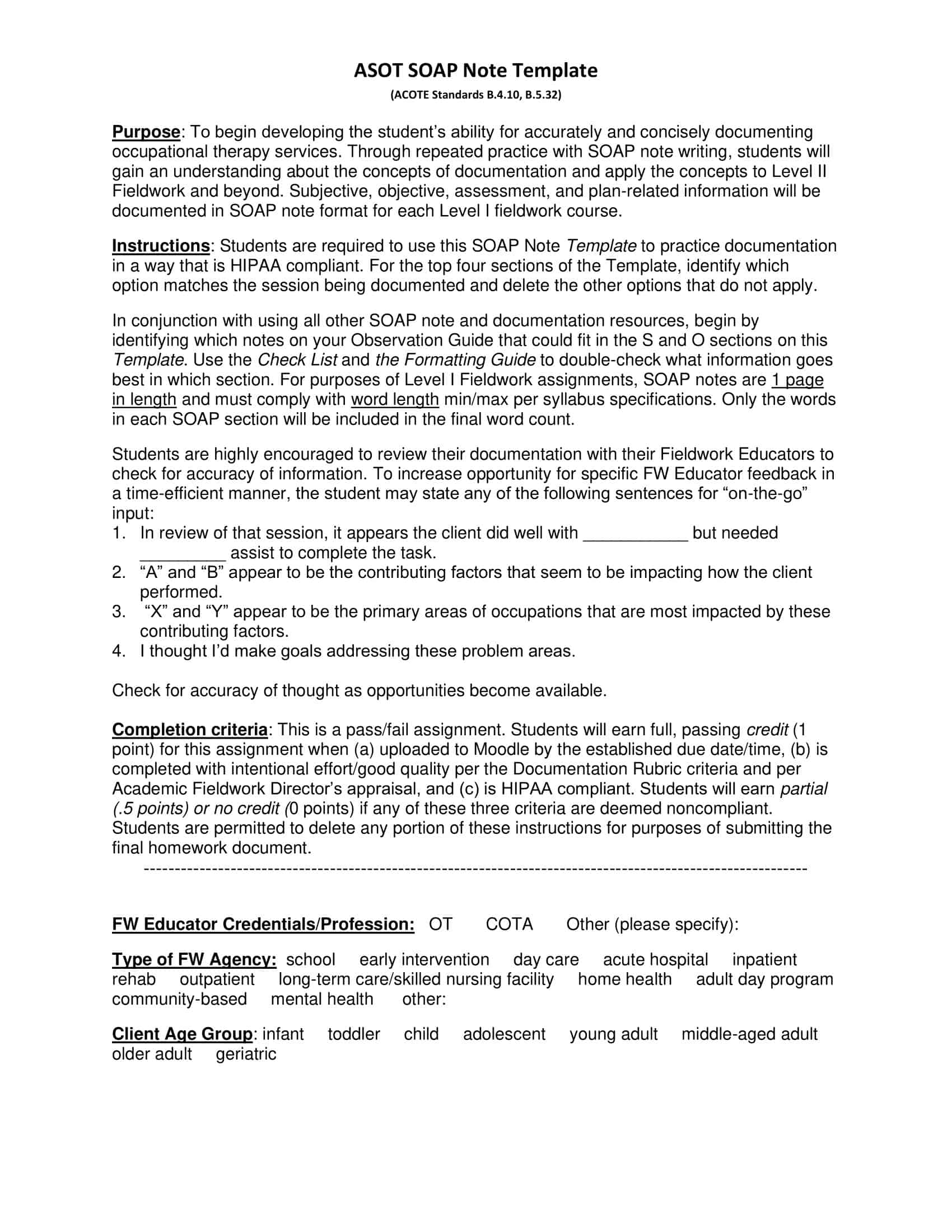
SOAP Note Templates are standardized forms used by healthcare professionals, such as doctors, nurses, and therapists, to document patient encounters and medical assessments in a structured and organized manner. SOAP stands for Subjective, Objective, Assessment, and Plan, which are the key components of a SOAP note. These templates ensure consistency, accuracy, and efficient record-keeping, allowing healthcare providers to effectively communicate and track patient information.
SOAP Note Templates provide a structured framework for healthcare providers to document patient encounters, ensuring that all necessary information is recorded consistently and comprehensively. These templates facilitate effective communication among healthcare professionals, continuity of care, and accurate documentation for legal and administrative purposes.
SOAP Note Templates are widely used in various healthcare settings, including hospitals, clinics, private practices, and outpatient facilities. By using these templates, healthcare providers can enhance their efficiency, improve patient care coordination, and maintain a systematic approach to documenting patient encounters and assessments.
History of Soap Notes

SOAP notes, also known as subjective, objective, assessment, and plan notes, have been used in the healthcare industry for many decades. The origins of SOAP notes can be traced back to the 1940s and 1950s, when the use of medical records began to increase in popularity. The development of SOAP notes was a response to the need for a more standardized and organized method of documenting patient information.
The first known use of the acronym SOAP in the medical field was by Dr. Lawrence Weed in the late 1960s. Dr. Weed, a physician and medical educator, developed the SOAP note as a method of organizing patient information and tracking progress in the treatment of patients. The SOAP note format was designed to be easy to use, quick to write, and easy to read. It was intended to be a simple, yet comprehensive method of documenting patient information.
The S in SOAP notes stands for subjective, which includes the patient’s symptoms, complaints, and history of the current illness. The O in SOAP notes stands for objective, which includes the physical examination findings and any relevant laboratory or imaging results.
The A in SOAP notes stands for assessment, which includes the physician’s interpretation of the patient’s symptoms, examination findings, and test results. The P in SOAP notes stands for plan, which includes the physician’s plan for the patient’s treatment, including any medications, referrals, or follow-up appointments.
The use of SOAP notes spread rapidly throughout the healthcare industry and became the standard method of documenting patient information in hospitals and clinics. Today, SOAP notes are used by a wide range of healthcare professionals, including physicians, nurses, physical therapists, and occupational therapists. They are used in a variety of settings, including hospitals, clinics, nursing homes, and private practice.
The use of electronic health records (EHRs) has also made SOAP notes more widely used. The use of EHRs, the electronic version of medical records, has made it easier to access, store, and share patient information. EHRs have also made it easier to use templates and pre-populated forms, which have made it even easier to create and use SOAP notes.
SOAP notes have been widely accepted as a valuable tool for healthcare professionals, providing a standardized and organized method of documenting patient information and tracking progress in the treatment of patients. They have been proven to be an essential tool for improving the quality of care provided to patients and for communication among healthcare professionals.
In conclusion, SOAP notes have been an essential tool in the healthcare industry for many decades. Developed by Dr. Lawrence Weed in the late 1960s, the SOAP note format was intended to be a simple, yet comprehensive method of documenting patient information. Today, SOAP notes are used by a wide range of healthcare professionals, in a variety of settings, and have been proven to be an essential tool for improving the quality of care provided to patients and for communication among healthcare professionals.
What is the benefit of using SOAP notes?
Writing SOAP notes can provide a number of benefits for healthcare professionals. Some of the main benefits include:
Improved patient care: SOAP notes can help healthcare professionals to document patient information and track progress in treatment, which can lead to improved patient care. By keeping accurate and comprehensive records, healthcare professionals can ensure that they are providing the best possible care to their patients.
Better communication: SOAP notes can also help to improve communication among healthcare professionals. By providing a standardized method of documenting patient information, SOAP notes can make it easier for healthcare professionals to share information and collaborate on patient care.
Increased efficiency: Writing SOAP notes can also increase efficiency in the healthcare setting. By providing a structured format for documenting patient information, SOAP notes can make it easier and quicker for healthcare professionals to document patient information and track progress in treatment.
Compliance with regulations: SOAP notes can also help healthcare professionals to comply with regulations related to patient care and documentation. By providing a standardized method of documenting patient information, SOAP notes can help healthcare professionals to meet regulatory requirements and avoid potential legal issues.
Evidence-based practice: SOAP notes can also help healthcare professionals to practice evidence-based medicine. By documenting patient information, symptoms, treatment plans, and outcomes, healthcare professionals can use the information in SOAP notes to evaluate the effectiveness of their treatment plans and make evidence-based decisions about patient care.
Better patient-provider relationship: SOAP notes can also help to improve the relationship between healthcare professionals and patients by providing a clear documentation of the patient’s condition, treatment plans and progress which can help in building trust and transparency between the two parties.
Essential Elements of SOAP Notes
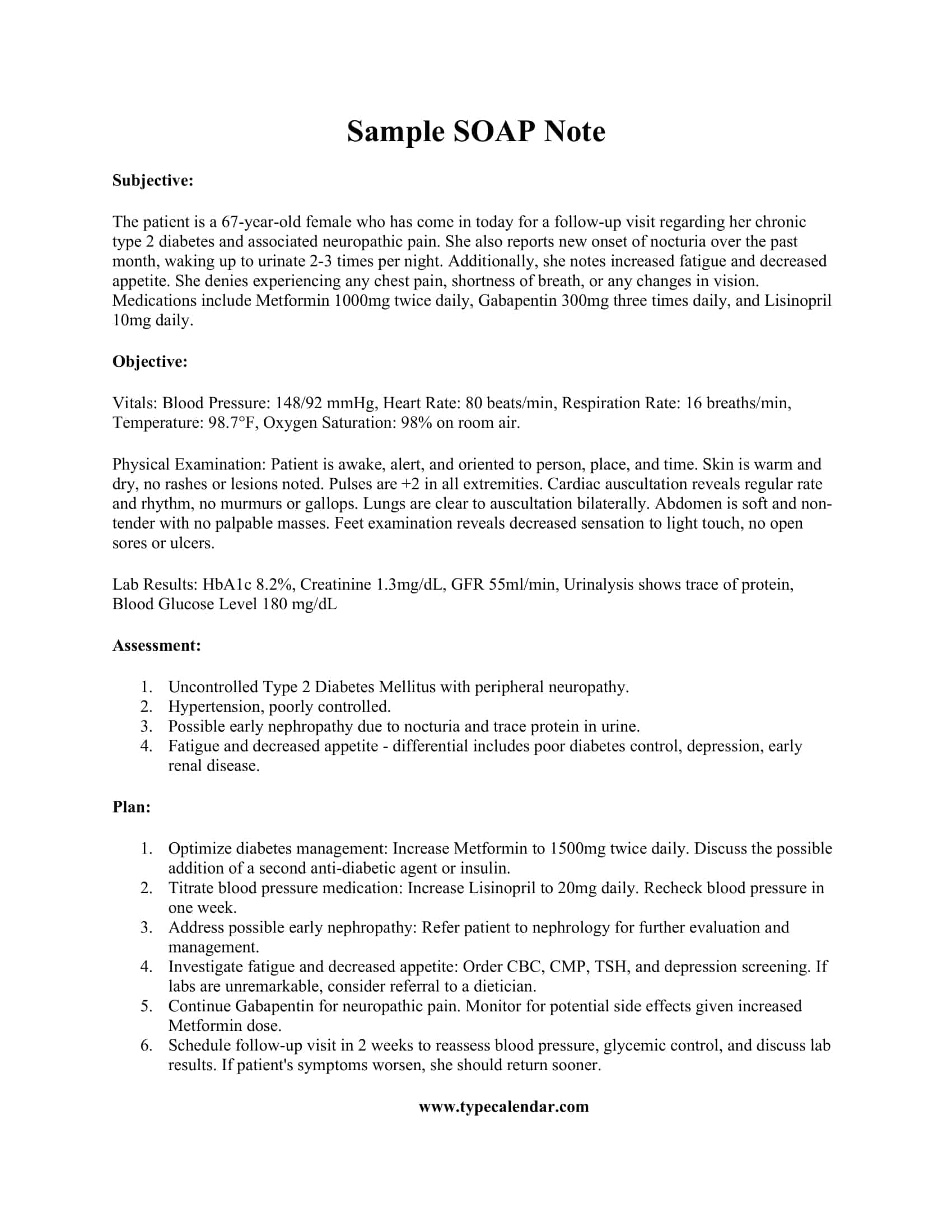
SOAP notes are a structured method of documenting patient information and are made up of four main elements:
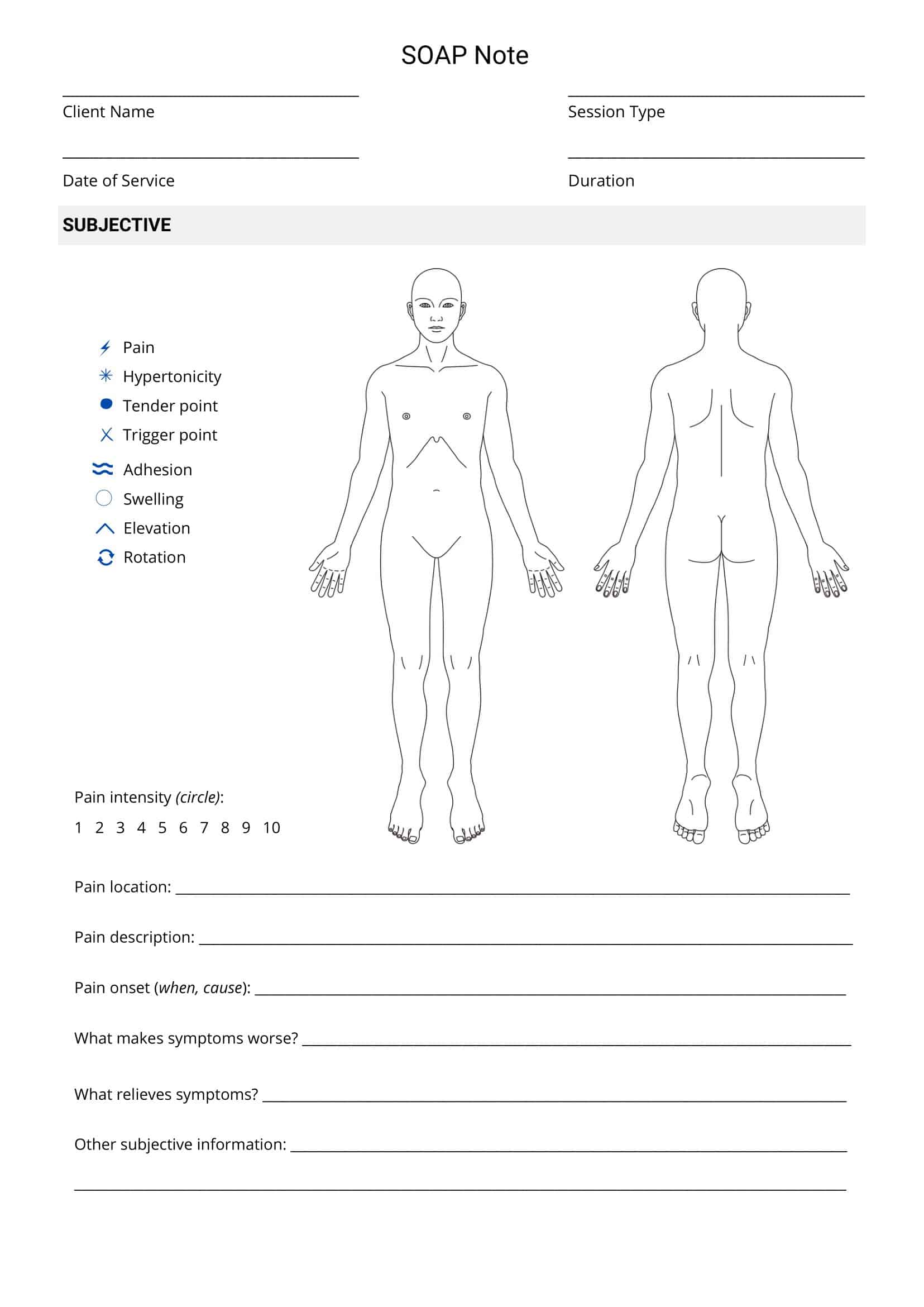
Subjective
This component includes information about the patient’s symptoms, complaints, and history of the current illness. This information is typically gathered through patient interviews, and it is written in the patient’s own words.
Objective
This component includes information about the physical examination findings and any relevant laboratory or imaging results. This information is typically gathered through examination and testing, and it is written in a factual, objective manner.
Assessment
This component includes the healthcare professional’s interpretation of the patient’s symptoms, examination findings, and test results. It also includes a diagnosis and any relevant information about the patient’s condition.
Plan
This component includes the healthcare professional’s plan for the patient’s treatment, including any medications, referrals, or follow-up appointments. It also includes any necessary instructions for the patient and any other relevant information about the patient’s care.
How to Write SOAP Notes
Writing SOAP notes is a process that involves several steps. Here is a guide on how to write SOAP notes:
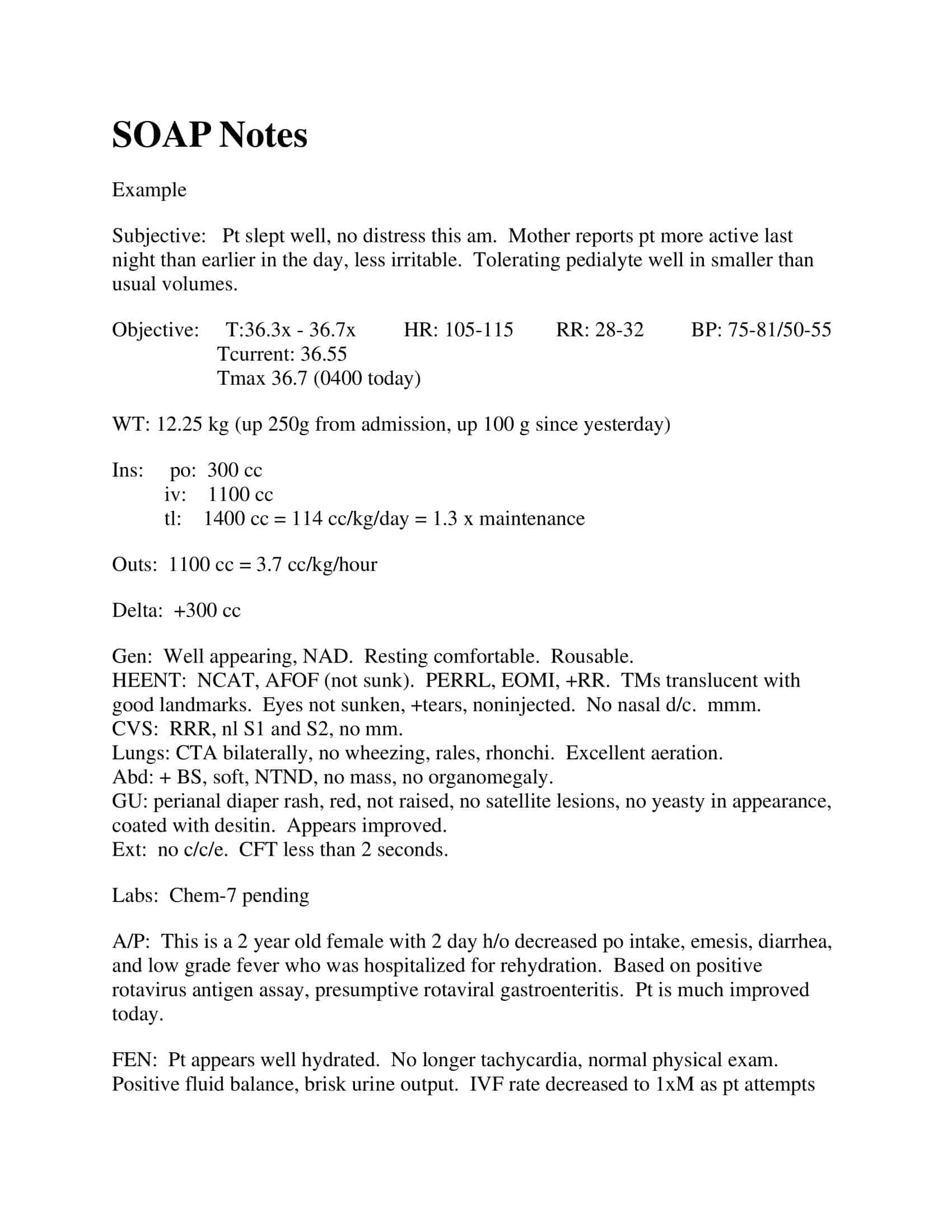
Gather patient information: Begin by gathering information about the patient’s symptoms, complaints, and history of the current illness. This information should be gathered through patient interviews and should be written in the patient’s own words.
Collect objective data: Collect information about the physical examination findings and any relevant laboratory or imaging results. This information should be gathered through examination and testing and should be written in a factual, objective manner.
Assess the patient: Analyze the patient’s symptoms, examination findings, and test results. Based on this information, make a diagnosis and write any relevant information about the patient’s condition.
Develop a plan: Develop a plan for the patient’s treatment, including any medications, referrals, or follow-up appointments. Also, include any necessary instructions for the patient and any other relevant information about the patient’s care.
Use a structured format: Use a structured format for documenting the patient information, such as the traditional SOAP format (Subjective, Objective, Assessment, Plan). Or use any other format that you find appropriate, like POMR (Problem-oriented medical record) or the DDx (differential diagnosis) format
Be concise and clear: Write your SOAP notes in a clear, concise, and professional manner. Use proper grammar and avoid using jargon or medical terms that may be difficult for others to understand.
Review and update: Review and update your SOAP notes regularly to ensure that the patient’s information is accurate and up to date. Keep in mind that SOAP notes are a legal document, thus should be written carefully.
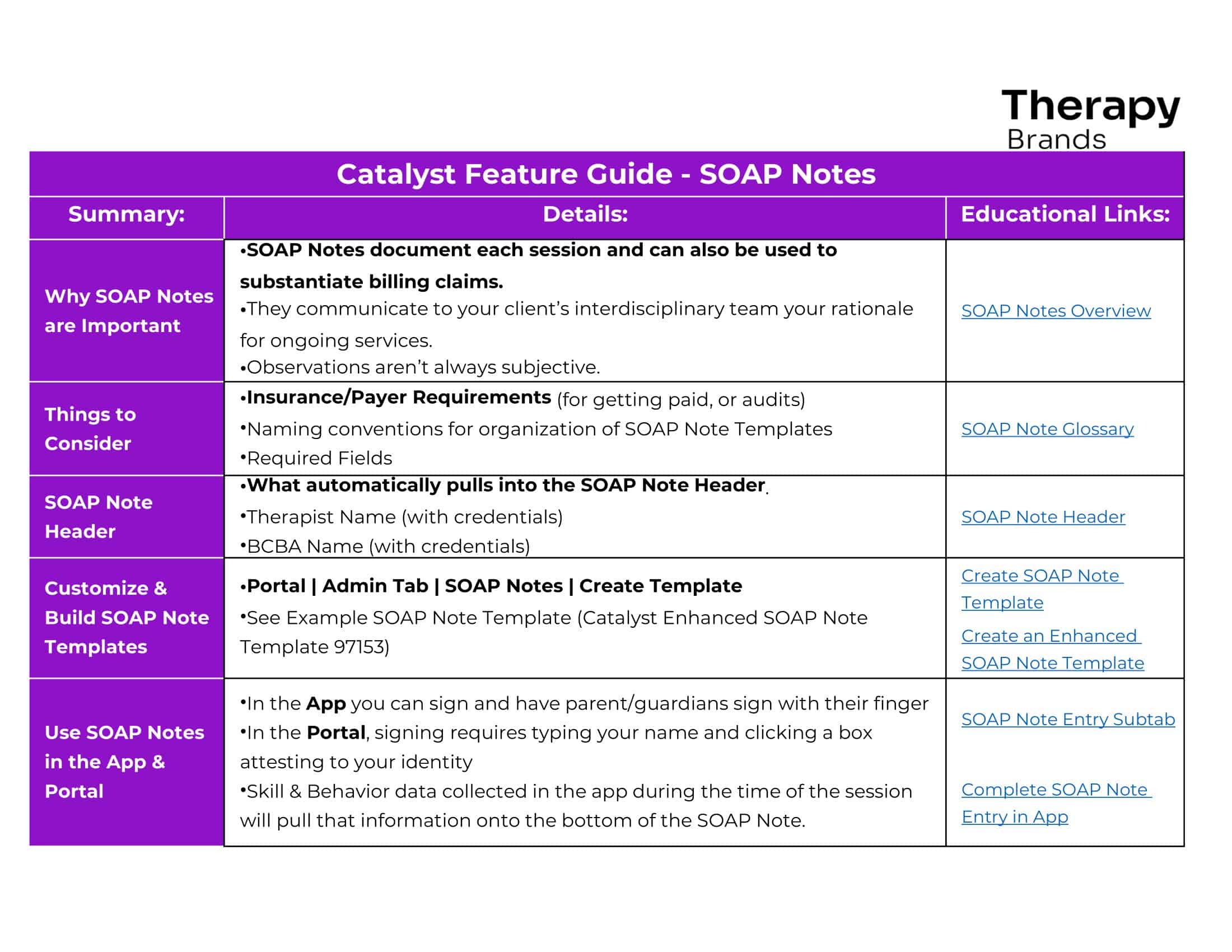
Use templates: Templates can help you to organize and structure your SOAP notes and make them more consistent. They can also help you to save time and focus on the most important information.
FAQs
Who uses SOAP notes?
SOAP notes are used by healthcare professionals in a variety of settings, including hospitals, clinics, nursing homes, and private practice. They are used by a wide range of healthcare professionals, including physicians, nurses, physical therapists, and occupational therapists.
How often should SOAP notes be written?
SOAP notes should be written every time a healthcare professional sees a patient. They should also be reviewed and updated regularly to ensure that the patient’s information is accurate and up to date.
Can SOAP notes be used in electronic health records (EHRs)?
Yes, SOAP notes can be used in electronic health records (EHRs). EHRs have made it easier to access, store, and share patient information, and they have also made it easier to use templates and pre-populated forms, which have made it even easier to create and use SOAP notes.
How do you structure a SOAP note?
SOAP notes document patient encounters following this structured format: S – Subjective observations like symptoms described O – Objective measurable assessments like exam findings A – Assessment diagnosis interpretation based on clinical impression P – Plan of treatment recommendations and next steps
What is the format for SOAP patient notes?
The SOAP format ensures patient notes systematically capture: S: Symptoms noticed by the patient
O: Clinical observations and facts by the provider A: Practitioner’s assessment of the diagnosis
P: Treatment plan details, medications, referrals
How do you make SOAP notes?
To make SOAP notes, compartmentalize details documented under corresponding sections:
S – Note verbatim symptoms reported.
O – Log vital signs, physical exam findings, lab results. A – Interpret findings into medical diagnoses. P – Outline treatment plans, orders, prescriptions and patient education.
How do I create a SOAP note template?
In a text editor or EHR fields, structure a template with designated sections for Subjective observations, Objective measurements, Assessment diagnosis interpretations, and Plan elements like medications, procedures, referrals – with sufficient space under each heading to capture details making SOAP notes quickly.
What is simple soap structure?
The simple SOAP structure stands for: S – Symptoms or Subjective Details
O – Objective Details A – Assessment or Analysis P – Plan Moving Forward
This format helps organize clear, concise progress notes.
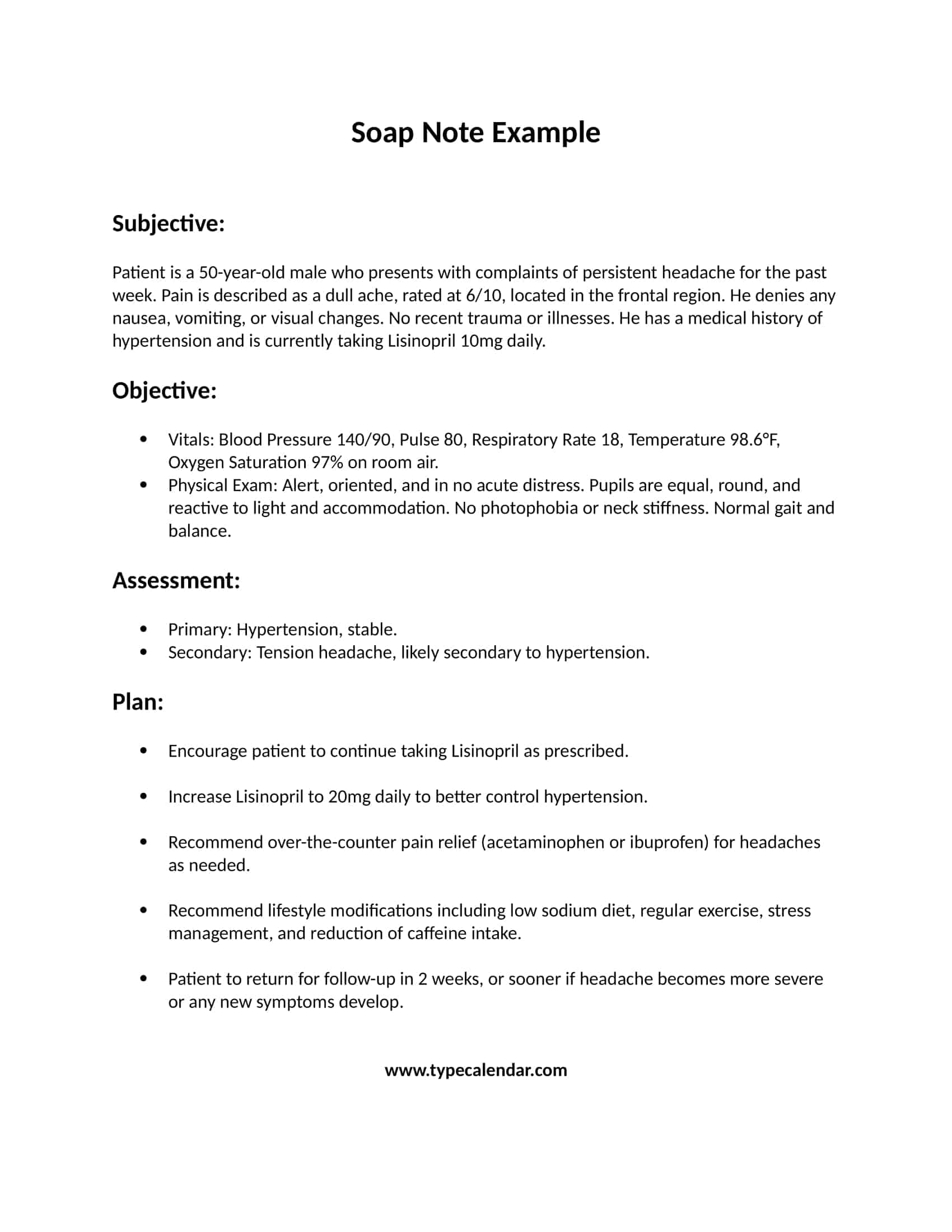
What is an example of a soap?
A SOAP note example:
S: Patient reports occasional migraines with visual aura lasting 4 hours.
O: Neurological exam normal, BP 132/84. CT ruled out abnormalities. A: Classic migraine diagnosis.
P: Prescribed Imitrex. Advised on trigger avoidance and sleep habits. Return in one month.


































![Free Printable Roommate Agreement Templates [Word, PDF] 1 Roommate Agreement](https://www.typecalendar.com/wp-content/uploads/2023/06/Roommate-Agreement-150x150.jpg)
![Free Printable Credit Card Authorization Form Templates [PDF, Word, Excel] 2 Credit Card Authorization Form](https://www.typecalendar.com/wp-content/uploads/2023/06/Credit-Card-Authorization-Form-150x150.jpg)
![Free Printable Stock Ledger Templates [Excel,PDF, Word] 3 Stock Ledger](https://www.typecalendar.com/wp-content/uploads/2023/08/Stock-Ledger-150x150.jpg)
