The SBAR (Situation-Background-Assessment-Recommendation) communication technique is a standardized method of effectively communicating important information about a patient’s condition or situation. It is widely used in healthcare settings to ensure that information is clearly and concisely conveyed between healthcare professionals, and is designed to facilitate clear and effective communication during critical or urgent situations.
The SBAR format provides a structured approach for organizing and presenting information, allowing for efficient and effective communication between team members, and helping to prevent misunderstandings or miscommunications that could lead to adverse outcomes. This article will provide an overview of the SBAR technique, including its purpose, components, and benefits, and will provide tips for effective use of the SBAR method in a healthcare setting.
Table of Contents
SBAR Templates
Enhance communication and collaboration in healthcare settings with our comprehensive collection of SBAR Templates. SBAR stands for Situation, Background, Assessment, and Recommendation—an effective framework for conveying critical information between healthcare professionals. Our customizable and printable templates provide a structured approach to communicate patient conditions, vital signs, medical history, and recommended actions.
By utilizing SBAR Templates, healthcare providers can ensure accurate and efficient handoffs, improve patient safety, and enhance the overall quality of care. With sections for each component of SBAR, our templates guide you through the process of organizing and delivering essential information in a concise and standardized manner. Streamline your communication, enhance patient outcomes, and foster a culture of effective teamwork with our user-friendly SBAR Templates. Download now and elevate the way you share information in healthcare settings.
What is the SBAR technique in nursing?

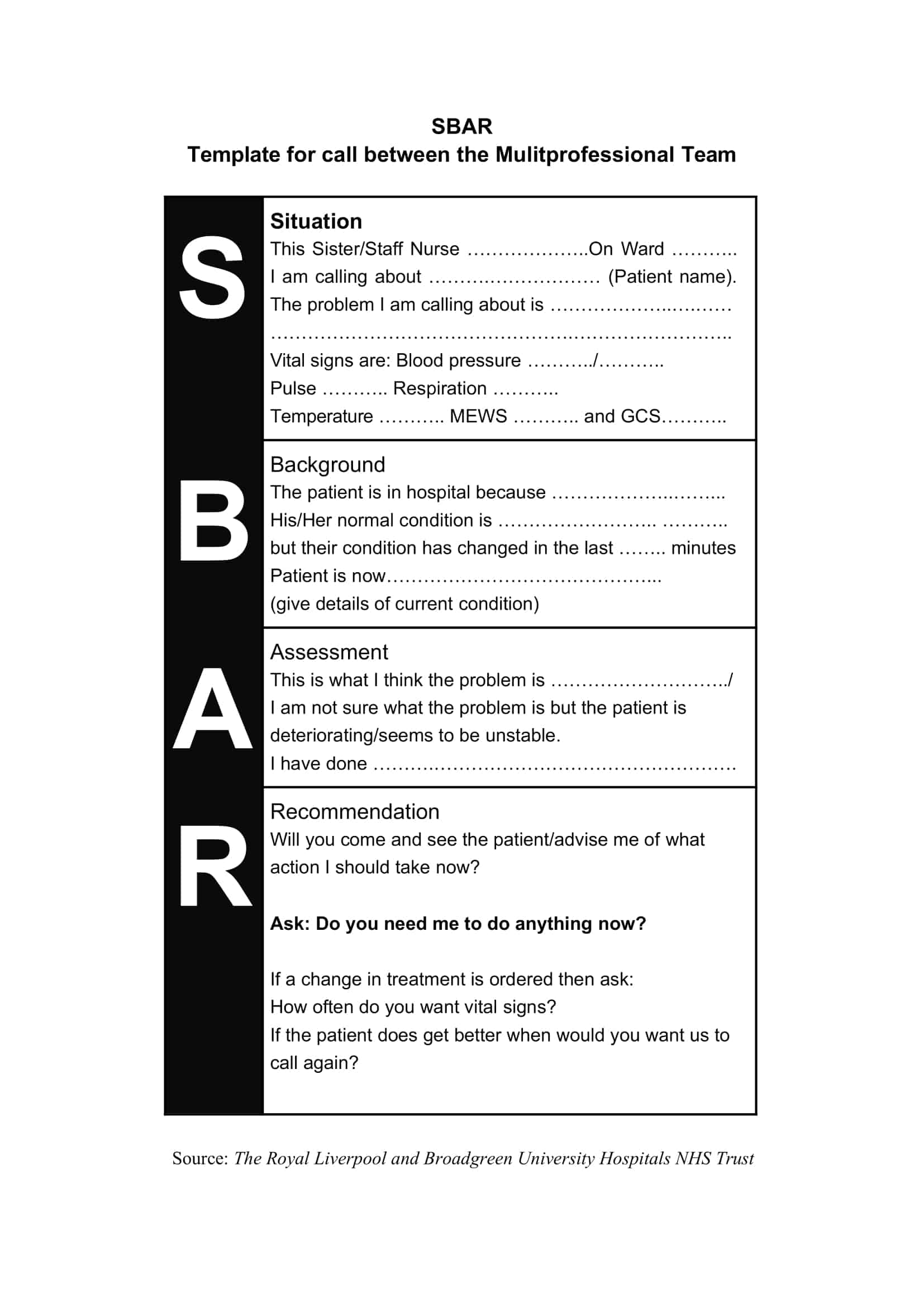
The SBAR (Situation-Background-Assessment-Recommendation) technique is a standardized method of communication used in healthcare to clearly and concisely convey important information about a patient’s condition or situation. The SBAR technique has four key components:
Situation: This section provides a brief and concise summary of the current situation or patient problem. It should include the patient’s name, location, and the nature of the problem.
Background: This section provides additional information about the patient’s history, including relevant medical history, current medications, and any previous treatment or procedures.
Assessment: This section presents a comprehensive evaluation of the patient’s condition, including a description of any vital signs, symptoms, or laboratory results, and an assessment of the patient’s overall condition.
Recommendation: This section outlines the recommended plan of action, including any necessary treatments, procedures, or referrals, and the rationale for these recommendations. It may also include any additional information or resources that are needed to ensure the best possible outcome for the patient.
The SBAR technique is used in healthcare settings to ensure effective communication between healthcare professionals and to prevent misunderstandings or miscommunications that could lead to adverse outcomes. By providing a standardized format for organizing and presenting information, the SBAR technique helps to ensure that critical information is effectively communicated and understood by all members of the healthcare team.
Benefits of SBAR technique in nursing
The SBAR technique offers several benefits for healthcare professionals, including:
Improved communication: The SBAR technique provides a standardized format for communicating important information, which helps to ensure that information is clearly and concisely conveyed between healthcare professionals. This reduces the risk of misunderstandings or miscommunications that could lead to adverse outcomes.
Increased efficiency: The SBAR technique provides a structured approach for organizing and presenting information, allowing for efficient and effective communication between team members. This can help to save time and reduce the risk of errors, improving overall patient care.
Enhanced patient safety: By providing a clear and concise summary of the patient’s situation, background, assessment, and recommendation, the SBAR technique helps to ensure that critical information is effectively communicated and understood by all members of the healthcare team. This can help to prevent adverse events and improve patient safety.
Improved teamwork and collaboration: The SBAR technique encourages active participation and collaboration between healthcare professionals, improving teamwork and fostering a culture of open communication.
Better documentation: The SBAR technique provides a clear and concise record of important information about a patient’s condition, which can be easily documented and referenced as needed. This can help to ensure that all relevant information is available and up-to-date, improving the quality of patient care.
When to use SBAR in nursing
The SBAR technique can be used in various situations in healthcare, including:
Report at shift change: The SBAR technique can be used to provide a concise and comprehensive summary of a patient’s condition and care plan at the start of a shift, allowing the incoming nurse to quickly and effectively understand the patient’s status and needs.
Emergencies or critical events: The SBAR technique can be used to communicate important information quickly and effectively during emergency or critical events, such as cardiac arrest or changes in a patient’s condition.
Interdisciplinary rounds: The SBAR technique can be used during interdisciplinary rounds, where healthcare professionals from different disciplines meet to discuss and review a patient’s care plan.
Consultations or referrals: The SBAR technique can be used when consulting with or referring a patient to another healthcare professional, allowing for clear and effective communication about the patient’s condition and needs.
Handoff of patient care: The SBAR technique can be used when transferring a patient from one healthcare provider to another, ensuring that all relevant information is effectively communicated and understood.
In any situation where clear and effective communication is critical to providing high-quality patient care, the SBAR technique can be used to ensure that important information is communicated and understood by all members of the healthcare team.
Important Tips for using SBAR in nursing
Here are some tips for using the SBAR technique effectively in nursing:
Practice using the SBAR format: Familiarizing yourself with the SBAR format and practicing using it in different scenarios can help you to become more comfortable and confident using the technique.
Keep it brief and to the point: The SBAR technique is designed to be a quick and effective way of communicating important information. Keep your communication brief and to the point, focusing on the most critical information.
Be clear and specific: When communicating important information, be clear and specific about what you are reporting. Avoid using vague or confusing terms, and provide relevant details and data to support your assessment and recommendations.
Use a calm and professional tone: The SBAR technique should be used in a calm and professional manner, avoiding the use of emotive or confrontational language. This can help to prevent misunderstandings or miscommunications and improve the effectiveness of the communication.
Encourage active listening: Encourage active listening and engagement from your colleagues by asking questions and clarifying any misunderstandings. This can help to ensure that all relevant information is communicated and understood.
Document the communication: Document the SBAR communication in the patient’s medical record to provide a clear and concise record of the patient’s status and care plan.
Train and educate team members: Ensure that all members of your healthcare team are trained and educated on the SBAR technique, including how to use it effectively and what information is critical to include.
Continuously evaluate and improve: Regularly evaluate the effectiveness of your SBAR communications and make changes as needed to improve the process. Encourage team members to provide feedback and suggestions for improvement.
Be flexible: While the SBAR format provides a structured approach to communication, be flexible and willing to modify it as needed to meet the specific needs of your patients and healthcare team.
Use SBAR as part of a comprehensive communication strategy: The SBAR technique should be used as part of a comprehensive communication strategy, alongside other tools and techniques such as handoff reports and huddle meetings.
How to write a perfect SBAR
The SBAR (Situation, Background, Assessment, and Recommendation) technique is a structured method of communicating important information between healthcare professionals. This technique can be used in a variety of situations, including during shift changes, emergencies, interdisciplinary rounds, consultations or referrals, and handoff of patient care. A well-written SBAR communication can help to improve patient safety and quality of care. Here is a step-by-step guide to writing a perfect SBAR:
Identify the situation
The first step in writing an SBAR is to identify the situation and what information needs to be communicated. This can include updates on a patient’s condition, changes in care plans, or any other relevant information.
Gather relevant information
Before beginning to write the SBAR, gather all relevant information about the patient, including their medical history, current condition, and any relevant test results. This information will be used to support your assessment and recommendations.
Begin with the situation
Start the SBAR by clearly stating the situation and providing a brief overview of what information needs to be communicated. This could be a simple statement such as “I need to provide an update on Mrs. Smith’s condition.”
Provide background information
The next step is to provide background information on the patient, including their medical history, current condition, and any relevant test results. This information will help to provide context for your assessment and recommendations.
Conduct a thorough assessment
In this section, conduct a thorough assessment of the patient’s condition, including a detailed evaluation of their symptoms and any relevant test results. This information will be used to support your recommendations.
Make recommendations
Based on your assessment, make clear and specific recommendations for the patient’s care, including any necessary changes to the care plan. This can include medication changes, diagnostic tests, or referrals to other healthcare professionals.
Document the SBAR
Once the SBAR is complete, document it in the patient’s medical record to provide a clear and concise record of the patient’s status and care plan.
Examples of SBAR in nursing
Here are some examples of SBAR in nursing:
Example 1
Situation: Update on a patient’s condition
Background: Mrs. Smith is a 65-year-old female admitted to the hospital for chest pain. She has a history of hypertension and heart disease.
Assessment: Mrs. Smith’s vital signs are as follows: blood pressure 160/100 mmHg, heart rate 92 bpm, and oxygen saturation 96% on room air. An ECG was performed and showed ST-segment elevation.
Recommendation: I recommend activating the Code STEMI protocol and transferring Mrs. Smith to the catheterization laboratory as soon as possible.
Example 2
Situation: Request for consultation
Background: Mr. Johnson is a 75-year-old male with a history of COPD who was admitted to the hospital for shortness of breath. He is currently on supplemental oxygen and antibiotics.
Assessment: Mr. Johnson’s respiratory status has worsened, and his oxygen saturation has dropped to 88% on 4 L/min of oxygen. A chest X-ray showed a right lower lobe infiltrate.
Recommendation: I request a consultation with the pulmonologist to evaluate Mr. Johnson for possible pneumonia and to discuss the need for intubation.
Example 3
Situation: Shift change report
Background: Mrs. Rodriguez is a 56-year-old female with a history of Type 2 diabetes admitted to the hospital for diabetic ketoacidosis. She received insulin therapy and fluid resuscitation, and her glucose level has stabilized.
Assessment: Mrs. Rodriguez is conscious and alert, her vital signs are stable, and her glucose level is 120 mg/dL.
Recommendation: I recommend continuing insulin therapy as per the order, monitoring vital signs every 4 hours, and administering oral fluids as tolerated.
Example 4
Situation: Request for assistance
Background: Mrs. Green is an 88-year-old female admitted to the hospital for a fall at home. She has a history of osteoporosis and dementia.
Assessment: Mrs. Green is confused and disoriented, and her vital signs are stable. She has developed a pressure ulcer on her sacrum.
Recommendation: I request assistance with repositioning Mrs. Green every 2 hours to prevent further deterioration of the pressure ulcer. I also recommend applying a new dressing and documenting the wound assessment in the medical record.
FAQs
How does the SBAR technique help to improve patient safety?
The SBAR technique helps to improve patient safety by reducing the risk of communication errors and improving the efficiency of information transfer. By using a structured and standardized format, the SBAR technique helps to ensure that important information is communicated accurately and effectively, reducing the risk of misunderstandings or missed information. This, in turn, helps to improve patient outcomes and reduce the risk of adverse events.
Can the SBAR technique be used in other healthcare settings besides nursing?
Yes, the SBAR technique can be used in other healthcare settings such as physician practices, ambulatory care centers, and long-term care facilities. The SBAR technique can be adapted for use by any healthcare professional who needs to communicate important patient information to other members of the healthcare team.
How can the SBAR technique be used to improve teamwork and collaboration among healthcare professionals?
The SBAR technique helps to improve teamwork and collaboration by providing a standardized format for communicating important information. By using a common language and format, healthcare professionals can more easily understand and interpret the information being communicated, leading to improved coordination and collaboration.
How can the SBAR technique be used to reduce the risk of medical errors?
The SBAR technique helps to reduce the risk of medical errors by improving the accuracy and efficiency of information transfer. By using a standardized format and language, healthcare professionals can ensure that important information is communicated clearly and accurately, reducing the risk of misunderstandings or missed information.
How can healthcare organizations implement the SBAR technique?
Healthcare organizations can implement the SBAR technique by providing training and education to all healthcare professionals on the proper use of the technique. Organizations can also develop standardized protocols and guidelines for using the SBAR technique in their facility, and encourage its use in daily practice. Regular assessments and audits can also be performed to monitor the effectiveness of the SBAR technique in improving communication and patient safety.
Is SBAR evidence-based?
Yes, the SBAR technique is considered to be evidence-based. It was developed based on research and best practices in healthcare communication and has been shown to improve the accuracy and efficiency of information transfer in numerous studies and real-world settings. The use of the SBAR technique has been associated with improved patient outcomes and reduced risk of adverse events, making it a valuable tool for healthcare professionals to improve patient safety.




































![Free Printable Roommate Agreement Templates [Word, PDF] 1 Roommate Agreement](https://www.typecalendar.com/wp-content/uploads/2023/06/Roommate-Agreement-150x150.jpg)
![Free Printable Credit Card Authorization Form Templates [PDF, Word, Excel] 2 Credit Card Authorization Form](https://www.typecalendar.com/wp-content/uploads/2023/06/Credit-Card-Authorization-Form-150x150.jpg)
![Free Printable Stock Ledger Templates [Excel,PDF, Word] 3 Stock Ledger](https://www.typecalendar.com/wp-content/uploads/2023/08/Stock-Ledger-150x150.jpg)
