Delving into the crossroads where medical necessity meets insurance coverage, we find a potent instrument – the ‘Letter of Medical Necessity‘ (LMN). This critical document, written by healthcare professionals, presents a compelling case for why certain treatments or services are indispensable for a patient’s health and recovery journey.
It’s the vital link that connects the clinical perspective with the financial considerations of insurance providers, transforming medical jargon into a comprehensive narrative that underscores the urgency and relevance of recommended medical interventions.
Table of Contents
What is a medical necessity letter?

A Letter of Medical Necessity (LMN) is a formal document written by a healthcare provider that outlines a patient’s specific medical needs and the reasoning behind a proposed course of treatment. This letter serves as a critical piece of evidence to justify the medical necessity of certain procedures, medications, or healthcare services.
Typically, an LMN is submitted to an insurance company or other payer to justify the need for a treatment or medication that may not typically be covered or is considered expensive. The letter outlines why the recommended care is essential for the patient’s health, often including details about the patient’s diagnosis, treatment history, and why alternative treatments are not suitable.
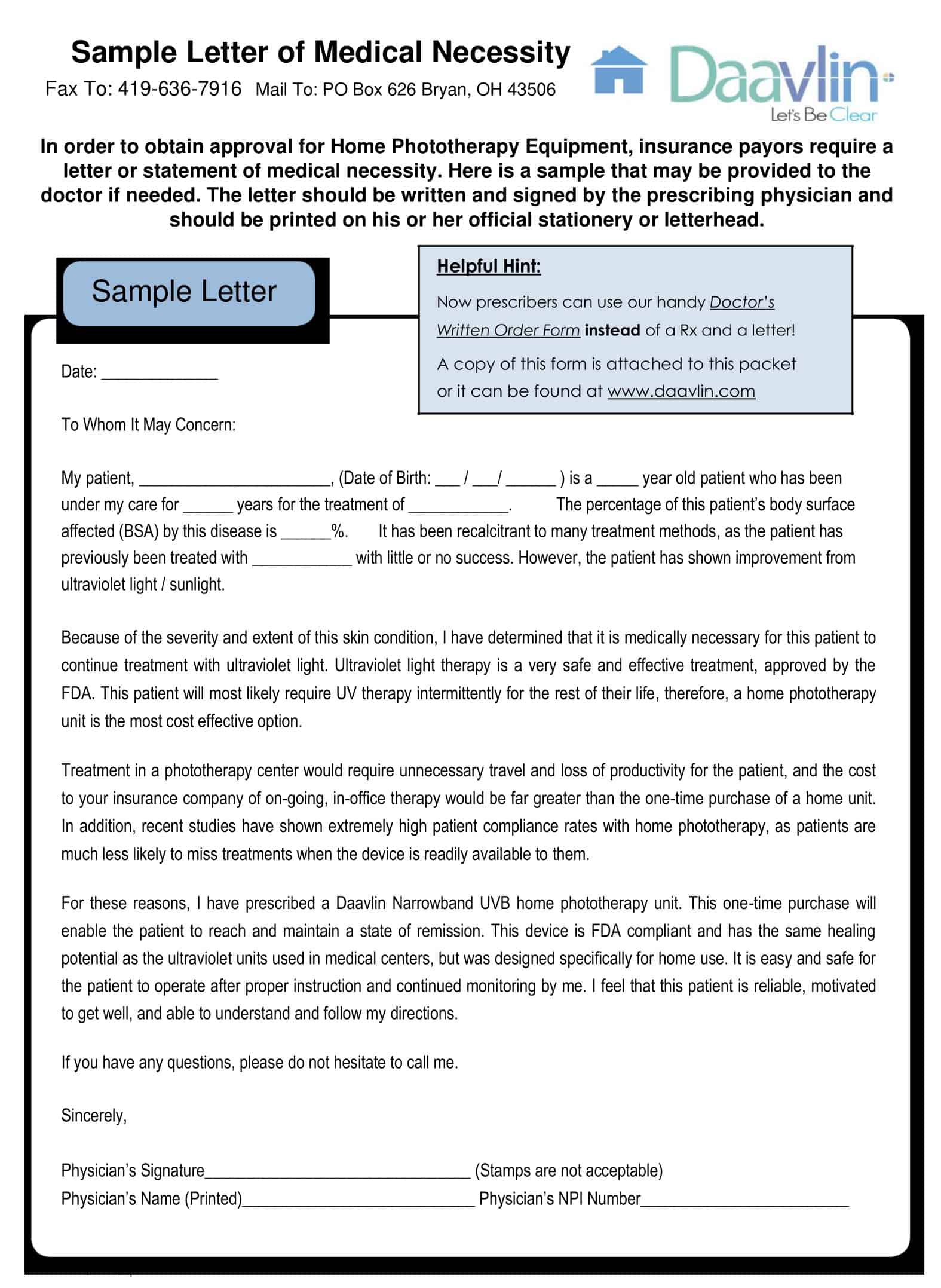
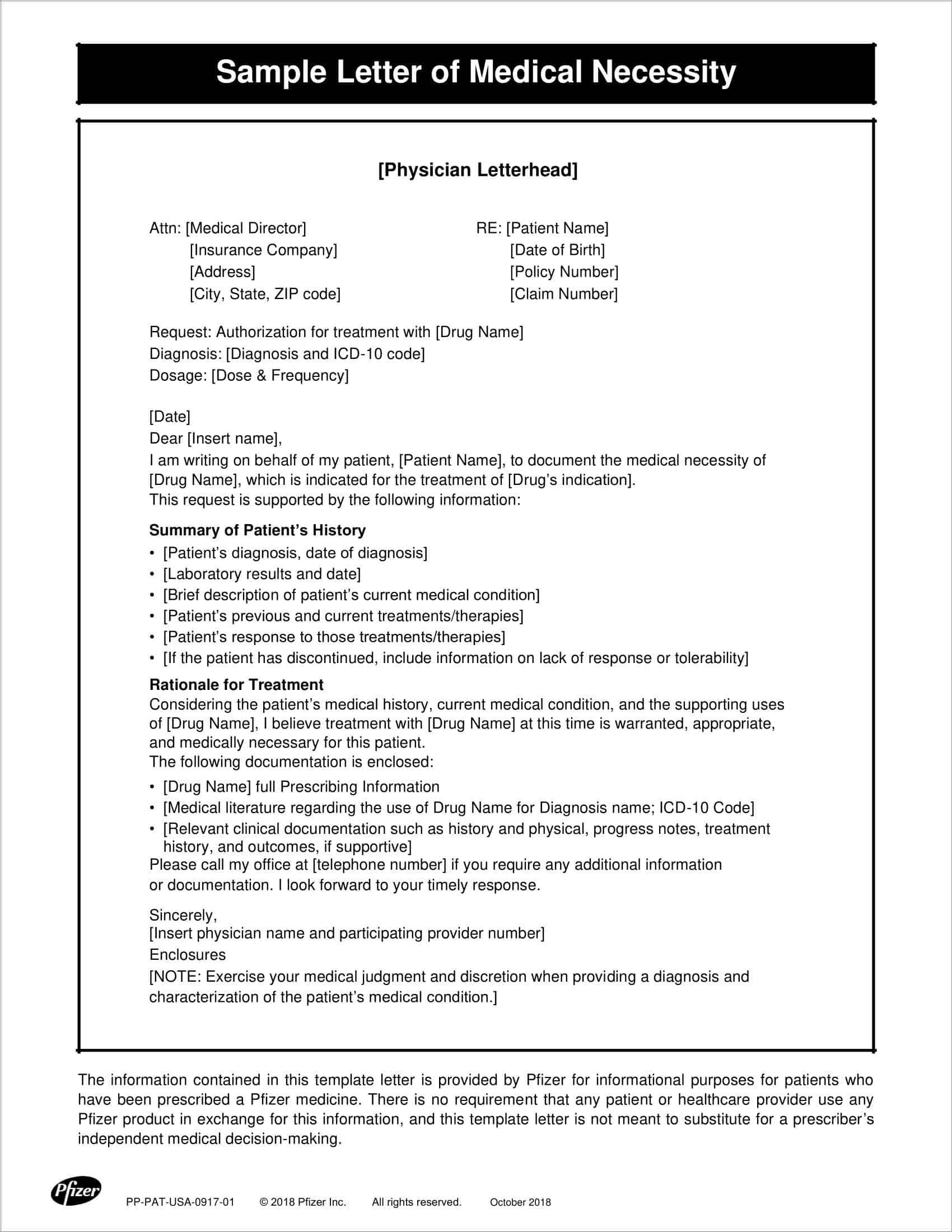
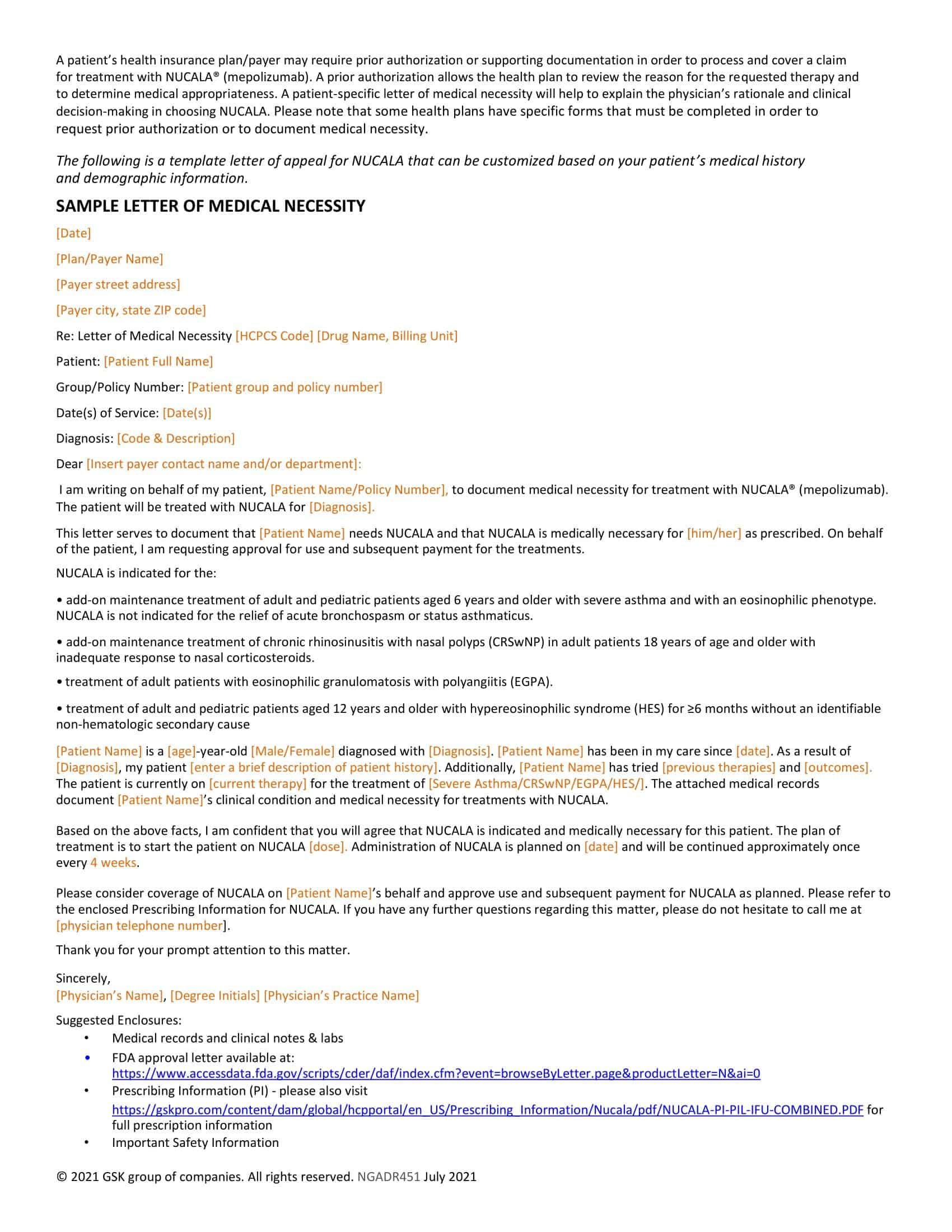
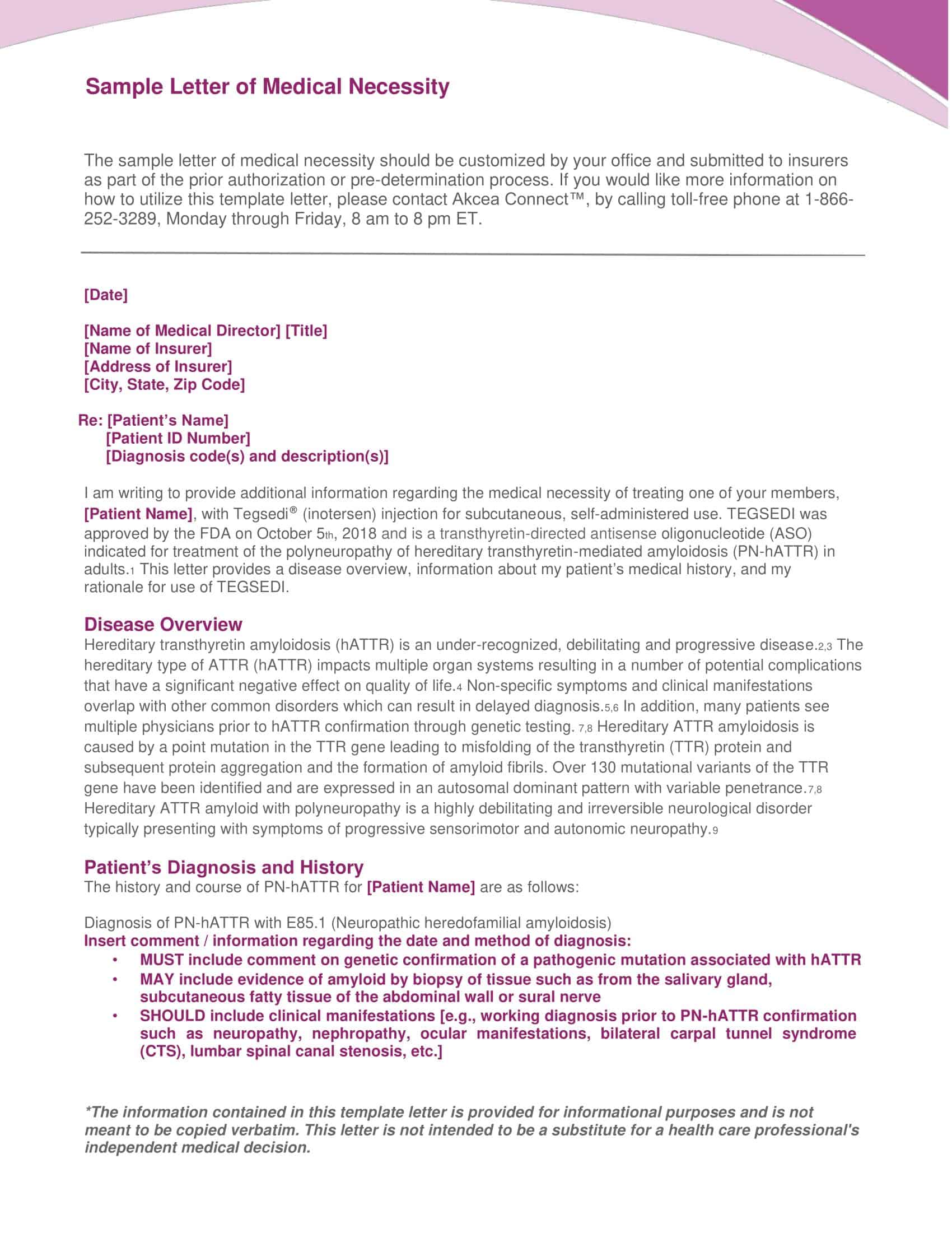
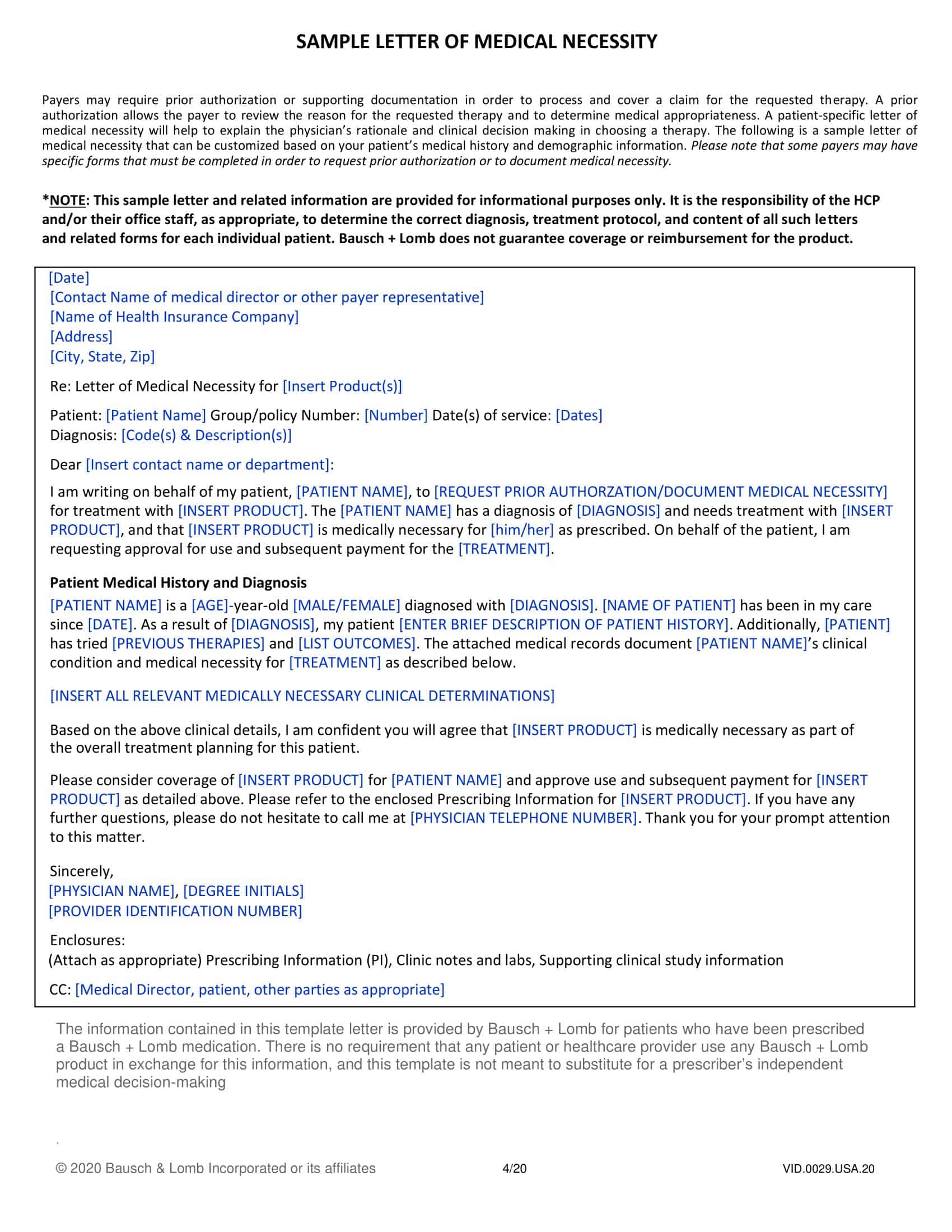
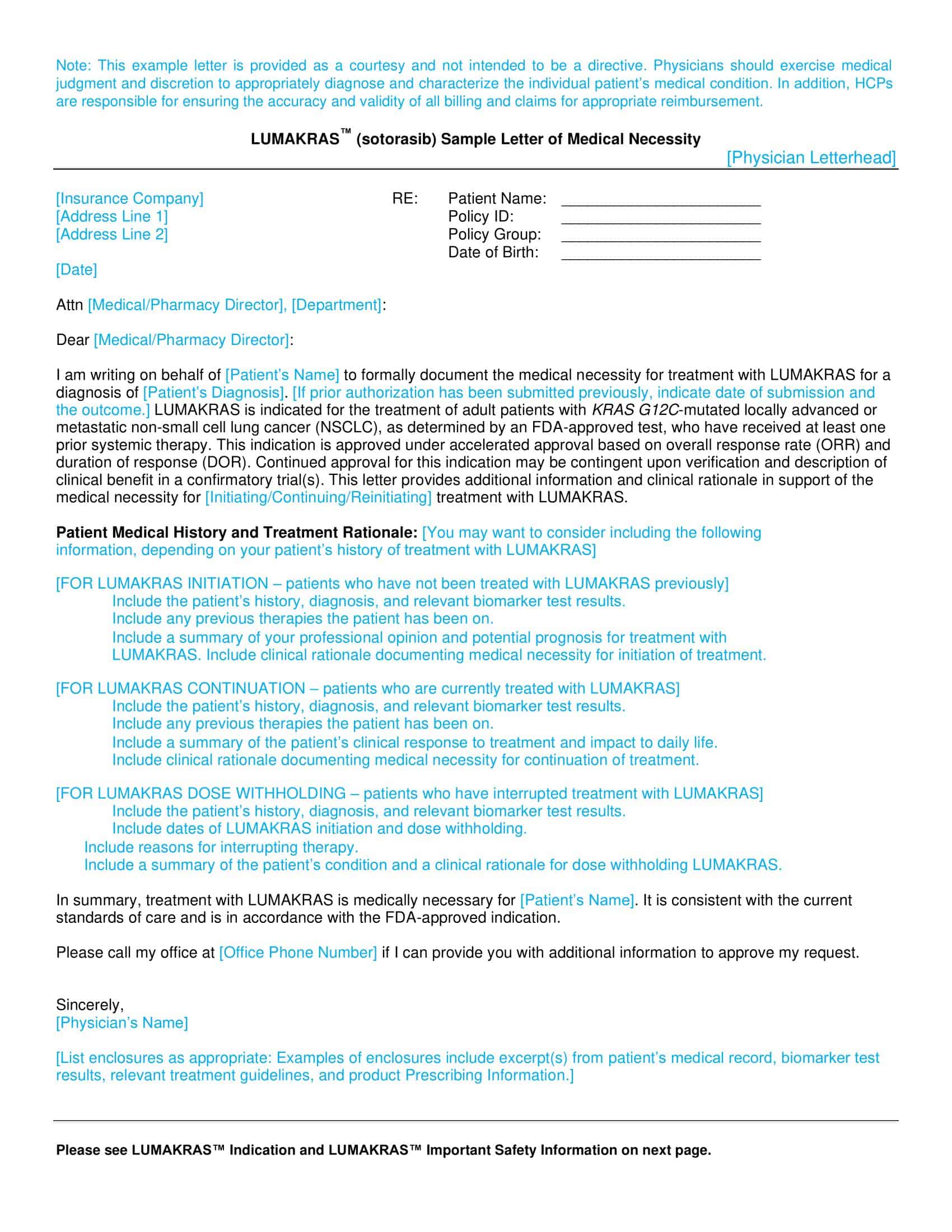
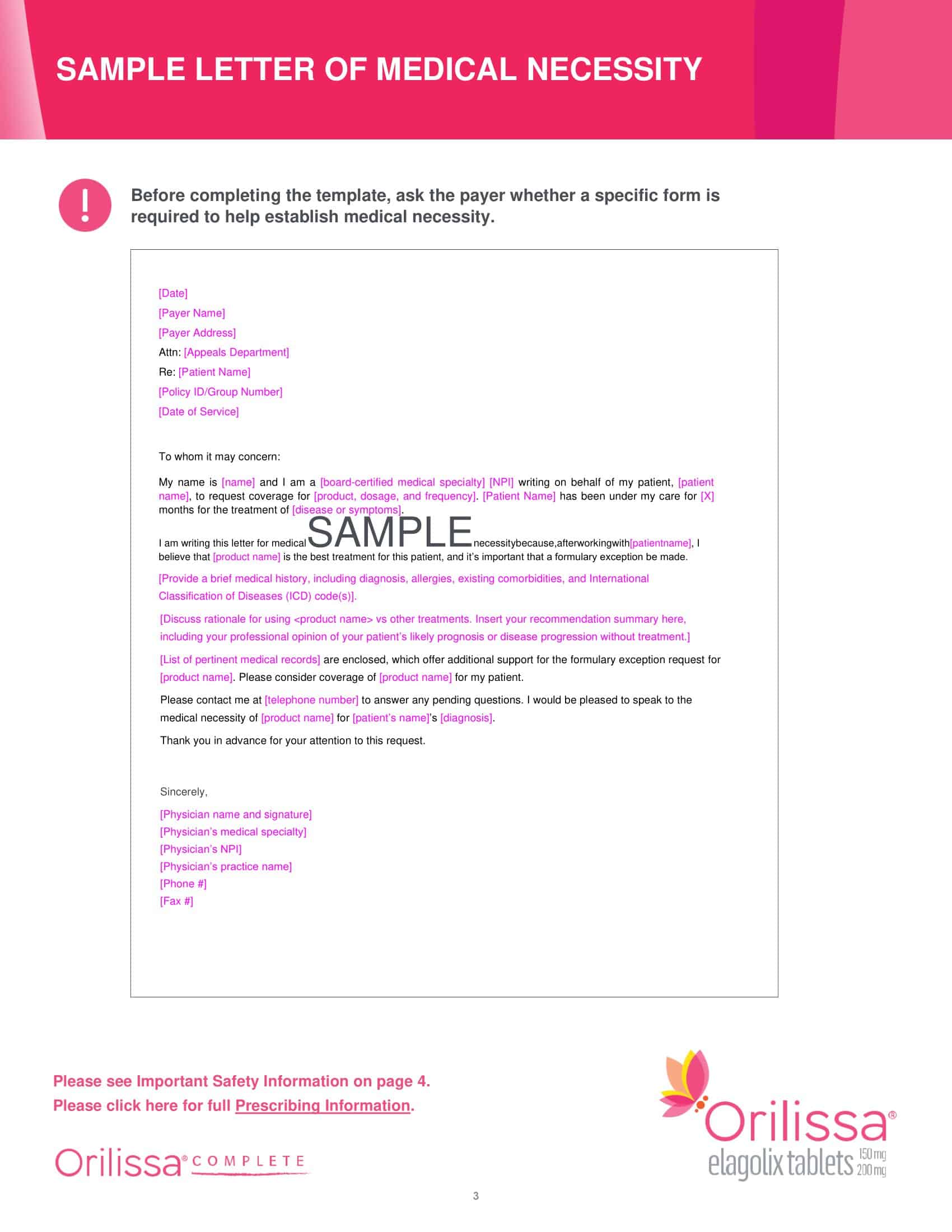
Letter Of Medical Necessity Templates
A Letter of Medical Necessity (LMN) is a crucial document used in healthcare to provide a detailed explanation of the medical need for a specific treatment, procedure, or medical equipment. It serves as a formal request to insurance providers, healthcare agencies, or other relevant parties, justifying the necessity and urgency of the requested medical intervention.
To ensure consistency and efficiency, healthcare professionals often utilize pre-designed templates for creating these letters. This comprehensive guide will delve into the specifics of Letter of Medical Necessity templates, their purpose, elements, and benefits.
Purpose of a letter of medical necessity
The purpose of a Letter of Medical Necessity (LMN) is multi-fold, but primarily it serves to validate the medical need for a specific treatment, medication, or service for a patient. Let’s delve into its core purposes and its importance within the healthcare and insurance landscapes:
Justifying Medical Need
An LMN is usually written by a healthcare provider to describe a patient’s medical condition and to assert the necessity of a specific medical treatment, equipment, or service. The letter explains in detail why this particular course of action is crucial for managing the patient’s health condition, or why it’s vital for their quality of life.
Facilitating Insurance Claims
The LMN is often used to help patients secure coverage for the cost of their healthcare needs from insurance companies. Since many insurance companies require proof of medical necessity for certain treatments or procedures, particularly those that are expensive or outside of standard protocols, the LMN serves as that proof.
Appealing Insurance Denials
In cases where coverage for a treatment, medication, or service has been denied by an insurance company, an LMN can serve as part of an appeal. By providing a detailed explanation of the medical necessity, an LMN can help overturn an initial denial of coverage.
Clarifying Unique Medical Scenarios
Sometimes, a patient’s condition may require a non-standard or innovative approach to treatment. In such cases, the medical necessity letter can explain why conventional treatment options are unsuitable, and why a unique or novel approach is needed.
Ensuring Continuity of Care
An LMN can also be used to advocate for the continuation of a specific treatment. For instance, if a patient is responding well to a particular drug that is typically only used short-term, a healthcare provider could use an LMN to explain the medical necessity of continuing this treatment long-term.
- The LMN is therefore not only a document stating a patient’s medical condition but also a well-formulated argument advocating for specific healthcare needs. It should contain detailed information including the patient’s diagnosis, the proposed treatment or service, the duration of the treatment, the provider’s information, why this treatment is medically necessary over other potential treatments, and how the treatment is expected to improve the patient’s condition.
When do you need a letter of medical necessity?
A Letter of Medical Necessity (LMN) is typically required under certain circumstances where there is a need to justify medical treatments, procedures, medications, or services. Here are several instances when an LMN is necessary:
Non-Standard or Non-Covered Treatment
If a patient requires a specific treatment or procedure that is not typically covered by their insurance plan, or is not seen as the standard course of treatment for their condition, an LMN is often necessary. The healthcare provider must explain why this treatment is the most appropriate option for the patient and how it is expected to benefit the patient’s health.
Special Medication Requirements
Some medications, especially those that are high-cost or experimental, may not be covered by insurance without further justification. In such cases, the LMN should outline why the medication is needed, why less expensive or standard medications aren’t suitable, and how the recommended medication will improve the patient’s condition.
Durable Medical Equipment (DME)
For equipment like wheelchairs, home oxygen equipment, or hospital beds to be covered by insurance, an LMN is usually required. The healthcare provider will need to detail why the equipment is medically necessary and how it will contribute to the treatment or management of the patient’s condition.
Non-Standard Diagnostic Tests
If a healthcare provider believes a specific diagnostic test that isn’t typically covered by insurance is crucial for diagnosing or managing a patient’s condition, they may need to provide an LMN. This letter should describe why the test is necessary and how its results will impact the treatment plan.
Insurance Claim Appeals
When an insurance claim has been denied, an LMN can be a powerful tool in the appeal process. The letter would need to provide additional medical justification for the service or treatment that was initially denied coverage.
Extended Care or Services
For treatments that are generally meant to be short-term but need to be extended for the patient’s wellbeing, an LMN could be necessary. The healthcare provider must explain why continuing the treatment is vital and how it contributes to the patient’s health status.
Special Dietary Needs
In some cases, prescribed diets or nutritional supplements may need to be justified through an LMN. This could include specialized infant formulas for babies with allergies or metabolic disorders, or nutritional supplements for patients with specific medical conditions.
- When an LMN is required, it should be detailed and clearly written, explaining the medical necessity of the prescribed treatment, medication, service, or equipment. This letter can significantly influence the decision-making process of insurance companies and help ensure that patients receive the care they need.
Key components of a medical necessity letter
A Letter of Medical Necessity (LMN) is a critical document within the healthcare industry. Its purpose is to outline the need for a specific treatment, procedure, or service and to convince an insurance company or other payer to cover the associated costs. Here are the key components that should be included in a well-crafted LMN:
Patient Information: Begin the letter with details about the patient. This should include the patient’s full name, date of birth, and insurance policy number.
Healthcare Provider Information: The letter should clearly state the name, credentials, contact information, and National Provider Identifier (NPI) of the healthcare provider.
Date: Include the date when the letter is written, as it’s important for record-keeping and potential future references.
Greeting: Address the letter to a specific individual if possible, otherwise use a general greeting such as ‘To Whom It May Concern.’
Introduction: The introduction should briefly explain the purpose of the letter, which is to establish the medical necessity for a specific treatment, medication, procedure, or piece of medical equipment.
Diagnosis: The diagnosis section should include a clear statement of the patient’s current medical condition, ideally including the relevant ICD-10 (International Classification of Diseases, Tenth Revision) codes.
Treatment Description: Clearly describe the proposed treatment, medication, procedure, or equipment that the patient needs. Include specifics such as the medication dosage, frequency of treatment, the type of equipment needed, etc.
Medical Necessity Explanation: This is the crux of the LMN. The healthcare provider should explain why the proposed treatment is medically necessary. This section should discuss why this specific treatment or procedure is required, how it will benefit the patient’s condition, and why alternatives are not suitable.
Supporting Evidence: Any supporting medical literature or studies that back up the need for the treatment can be mentioned. This section helps reinforce the medical justification for the requested procedure or treatment.
Duration: Indicate the length of time the patient will need the treatment, medication, or equipment.
Conclusion: In the closing section, request the insurance company or payer to cover the cost of the proposed treatment due to its medical necessity for the patient’s condition.
Signature: The healthcare provider should sign the letter, reinforcing their professional authority and the credibility of the contents of the letter.
Which items typically necessitate a letter of medical justification?
Here are items that typically require a letter of medical necessity:
- Durable Medical Equipment (wheelchairs, hospital beds, oxygen equipment, etc.)
- Special Medications (expensive drugs, non-formulary or off-label use drugs)
- Prosthetic Devices (artificial limbs, breast prostheses, cochlear implants, etc.)
- Orthotic Devices (braces, splints, artificial eyes, etc.)
- Physical Therapy
- Occupational Therapy
- Speech Therapy
- Home Health Care
- Specialized Surgeries (bariatric surgery, cosmetic surgery for medical reasons, etc.)
- Experimental or Non-traditional Treatments
- Mental Health Services (psychotherapy, residential treatment, etc.)
- Specialized Medical Foods (for inborn errors of metabolism)
- Certain Vaccines (travel vaccines, etc.)
- Genetic Testing
- Rehabilitative Services
- Chronic Pain Management Treatments (nerve blocks, acupuncture, etc.)
- Assistive Technology (communication devices for non-verbal patients, etc.)
- Specialized Diagnostic Testing (PET scans, genetic tests, etc.)
- Long-term Care Services
- Ambulance or Medical Transportation Services.
Who is responsible for writing a letter of medical necessity?
The primary responsibility for writing a Letter of Medical Necessity rests with the healthcare provider, usually a doctor or specialist who is familiar with the patient’s medical history and current health condition. The healthcare provider must be able to provide a detailed explanation and justification for the medical necessity of the proposed treatment or procedure.
How to write letter of medical necessity
Here’s a detailed step-by-step guide on how to write a Letter of Medical Necessity:
Step 1: Letterhead and Date
The letter should be written on professional letterhead if available, indicating the medical professional’s contact information and the date. If letterhead is not available, make sure to include this information at the top of the document.
Step 2: Patient Identification
Identify the patient. Include their full name, date of birth, insurance policy number, and other identifying information as appropriate.
Step 3: Recipient Address
Include the recipient’s address. This will typically be the insurance company or a specific department within the company. Make sure to find the correct address to avoid delays.
Step 4: Introduction
Begin the body of the letter by stating your purpose. This should include a brief introduction of yourself as the healthcare provider, your relationship with the patient, and the specific purpose of the letter – to establish medical necessity for a particular procedure, treatment, or device.
Step 5: Description of Patient’s Condition
Describe the patient’s current health condition. This should include any diagnoses, symptoms, and how these impact the patient’s daily life or functionality. Use clear, straightforward language that a layperson can understand, while also providing enough medical detail to justify the medical necessity.
Step 6: Previous Treatments
Detail the previous treatments, procedures, or devices that have been attempted, including their outcomes. If those were ineffective or had limited effect, this can help establish the necessity for the treatment you’re recommending.
Step 7: Proposed Treatment and Medical Necessity Justification
Clearly state the recommended treatment, procedure, or device and explain why it is medically necessary for the patient’s condition. Use scientific evidence, clinical guidelines, or consensus statements where possible to back up your claim. Explain how this treatment will improve the patient’s health condition or quality of life.
Step 8: Potential Consequences
Explain the potential consequences if the patient does not receive the proposed treatment, procedure, or device. This could include worsening of symptoms, reduced quality of life, or development of more serious health issues.
Step 9: Closing Statement
End the letter by summarizing the patient’s need for the proposed treatment and your professional recommendation. This is also a good place to invite further communication or questions from the insurance company.
Step 10: Signature
Finally, the healthcare provider should sign the letter, indicating their professional role, degree or credentials.
A sample letter of medical necessity
[Your Name]
[Your Title]
[Your Institution Name]
[Your Institution Address]
[City, State, ZIP]
[Email Address]
[Phone Number]
[Date]
[Insurance Company Name]
[Insurance Company Address]
[City, State, ZIP]
Re: [Patient’s Full Name]
DOB: [Patient’s Date of Birth]
Policy Number: [Patient’s Policy Number]
Dear [Claims Reviewer’s Name],
I am writing to you as the treating physician of [Patient’s Full Name], to provide clinical information in support of medical necessity for [the treatment, procedure, or medical device in question].
Mr./Ms. [Patient’s Last Name] has been diagnosed with [Patient’s Diagnosis], an ongoing condition that significantly impacts their quality of life. The symptoms of [Patient’s Diagnosis] have been severe and debilitating, including [symptoms or functional limitations the patient experiences related to their diagnosis].
We have tried various other treatment options, including [List previous treatments and their outcomes, such as: “Medications A, B, and C, physical therapy, and occupational therapy”]. Despite these efforts, the symptoms of [Patient’s Diagnosis] persist, thereby severely affecting [Patient’s First Name]’s daily life and activities.
After careful consideration and review of their medical history, I am recommending [the treatment, procedure, or medical device in question] as it offers the best potential for managing [Patient’s First Name]’s condition. [Here, provide medical justification for the procedure or device. For example: “Numerous studies indicate that Treatment X is effective in reducing symptoms of Condition Y and improving patients’ quality of life.”]
Without [the treatment, procedure, or medical device in question], [Patient’s First Name] is likely to experience [potential consequences of not receiving the recommended treatment, such as: “an increase in symptom severity, further functional limitations, or a decrease in quality of life”].
Considering the severity of [Patient’s First Name]’s condition and the lack of response to other treatment options, it is crucial that [Patient’s First Name] receives [the treatment, procedure, or medical device in question] as soon as possible. I am confident that this course of action will help improve [Patient’s First Name]’s condition and quality of life.
Please feel free to contact me if you require additional information or clarification on this matter. Thank you for considering this request for [the treatment, procedure, or medical device in question] for [Patient’s Full Name].
Sincerely,
[Your Name]
[Your Title]
[Your Signature]
FAQs
How long should a Letter of Medical Necessity be?
The length of a Letter of Medical Necessity can vary depending on the complexity of the medical condition and the treatment being requested. It should be concise and focused while including all the necessary information to support the medical necessity. Typically, it ranges from one to three pages.
Can a patient write a Letter of Medical Necessity?
In most cases, a patient cannot write a Letter of Medical Necessity. It is usually written by a healthcare professional who has the medical expertise and knowledge to provide a detailed and clinically sound explanation for the requested treatment or intervention. However, the patient’s input and personal experiences can be valuable in assisting the healthcare professional in crafting an effective letter.
Is a Letter of Medical Necessity always required for insurance coverage?
Not all medical treatments, procedures, medications, or devices require a Letter of Medical Necessity for insurance coverage. The necessity for a letter depends on the specific requirements and policies of the insurance provider or healthcare payer. Some routine or commonly covered medical interventions may not require a letter, while others, especially those considered experimental or non-standard, may require strong justification.
Can a Letter of Medical Necessity guarantee insurance coverage or reimbursement?
While a well-written Letter of Medical Necessity can significantly increase the chances of obtaining insurance coverage or reimbursement, it does not guarantee approval. The final decision lies with the insurance company or healthcare payer, who considers various factors, including policy limitations, medical evidence, and their own review processes.
Are there specific templates available for writing a Letter of Medical Necessity?
While there are no universal templates for a Letter of Medical Necessity, some healthcare providers or insurance companies may provide their own templates or guidelines. It’s important to follow any specific instructions or requirements provided by the entity to which the letter is being submitted. However, the content and structure of the letter should always be tailored to the specific medical condition, treatment, or device being requested.
Can a Letter of Medical Necessity be used for appeals?
Yes, a Letter of Medical Necessity can be used as part of the appeals process if an initial request for coverage or reimbursement is denied. In an appeal, the letter can be supplemented with additional supporting documentation or updated information to strengthen the case for medical necessity. The requirements and procedures for appeals may vary depending on the insurance provider or healthcare payer.
Is there a deadline for submitting a Letter of Medical Necessity?
The deadline for submitting a Letter of Medical Necessity depends on the specific requirements and policies of the insurance provider or healthcare payer. It’s essential to review the instructions or guidelines provided by the entity and submit the letter within the specified timeframe. Missing the deadline could result in a delay or denial of coverage.
Can a Letter of Medical Necessity be used for tax purposes?
A Letter of Medical Necessity is primarily used for insurance coverage or reimbursement purposes rather than tax purposes. However, in some cases, the information provided in the letter may be used to support claims for medical expenses when filing taxes. It’s important to consult with a tax professional or refer to relevant tax regulations in your jurisdiction for specific guidelines regarding medical expense deductions.
Can a Letter of Medical Necessity be used for requesting accommodations or services in educational or workplace settings?
While a Letter of Medical Necessity primarily relates to insurance coverage and reimbursement, similar documentation, such as a medical statement or letter from a healthcare professional, may be required to request accommodations or services in educational or workplace settings. These requests are typically handled through separate processes governed by educational institutions or employers and may require specific forms or documentation.
Can a Letter of Medical Necessity be used for obtaining disability benefits?
A Letter of Medical Necessity may be one of the supporting documents required when applying for disability benefits. The specific requirements and forms vary depending on the disability benefits program and the country in which you reside. It’s advisable to consult with the relevant disability benefits agency or seek legal advice to understand the specific documentation needed for a disability benefits application.




































![Free Printable Friendly Letter Templates [PDF, Word, Excel] 1st, 2nd, 4th Grade 1 Friendly Letter](https://www.typecalendar.com/wp-content/uploads/2023/05/Friendly-Letter-150x150.jpg 150w, https://www.typecalendar.com/wp-content/uploads/2023/05/Friendly-Letter-1200x1200.jpg 1200w)
![%100 Free Hoodie Templates [Printable] +PDF 2 Hoodie Template](https://www.typecalendar.com/wp-content/uploads/2023/05/Hoodie-Template-1-150x150.jpg)
![43+ Printable Leave of Absence Letter (LOA) Templates [PDF, Word] / Free 3 Leave of Absence Letter](https://www.typecalendar.com/wp-content/uploads/2023/01/Leave-of-Absence-Letter-150x150.jpg 150w, https://www.typecalendar.com/wp-content/uploads/2023/01/Leave-of-Absence-Letter-1200x1200.jpg 1200w)
