Whenever you attend a therapy session, you might observe the therapist taking notes periodically. As you engage in conversation and respond to their inquiries, they diligently document key details. Although this might cause unease for some individuals, there is no cause for concern.
The therapist aims to gain a deeper understanding of your situation in order to provide effective support. With various factors possibly contributing to your decision to seek therapy, they strive to offer valuable assistance. By maintaining a record of your sessions, they establish a foundation for future progress. It is perfectly natural to feel inquisitive and seek clarification on the purpose of these notes.
Table of Contents
What are Therapy Notes?

Therapy notes, also known as progress notes or case notes, are written records created by therapists during or after a therapy session. These notes serve as a documentation of the client’s progress, the therapist’s observations, and the interventions used throughout the therapeutic process. They typically include information about the client’s symptoms, emotions, behaviors, and responses to treatment, as well as any goals and plans for future sessions.
Therapy notes are an essential tool for therapists as they help track progress, facilitate communication with other healthcare professionals, and ensure continuity of care. Additionally, they are often required for legal, ethical, and insurance-related purposes.
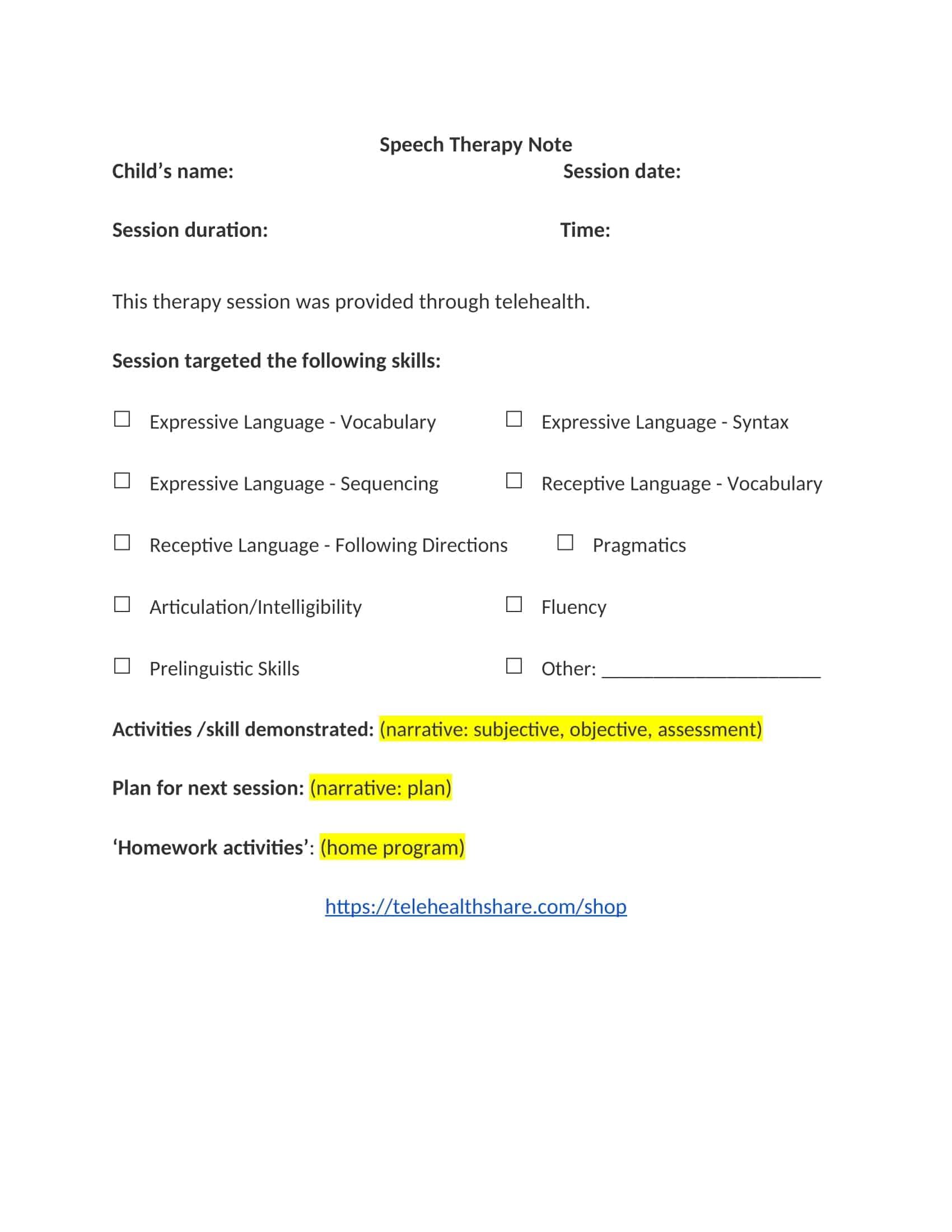
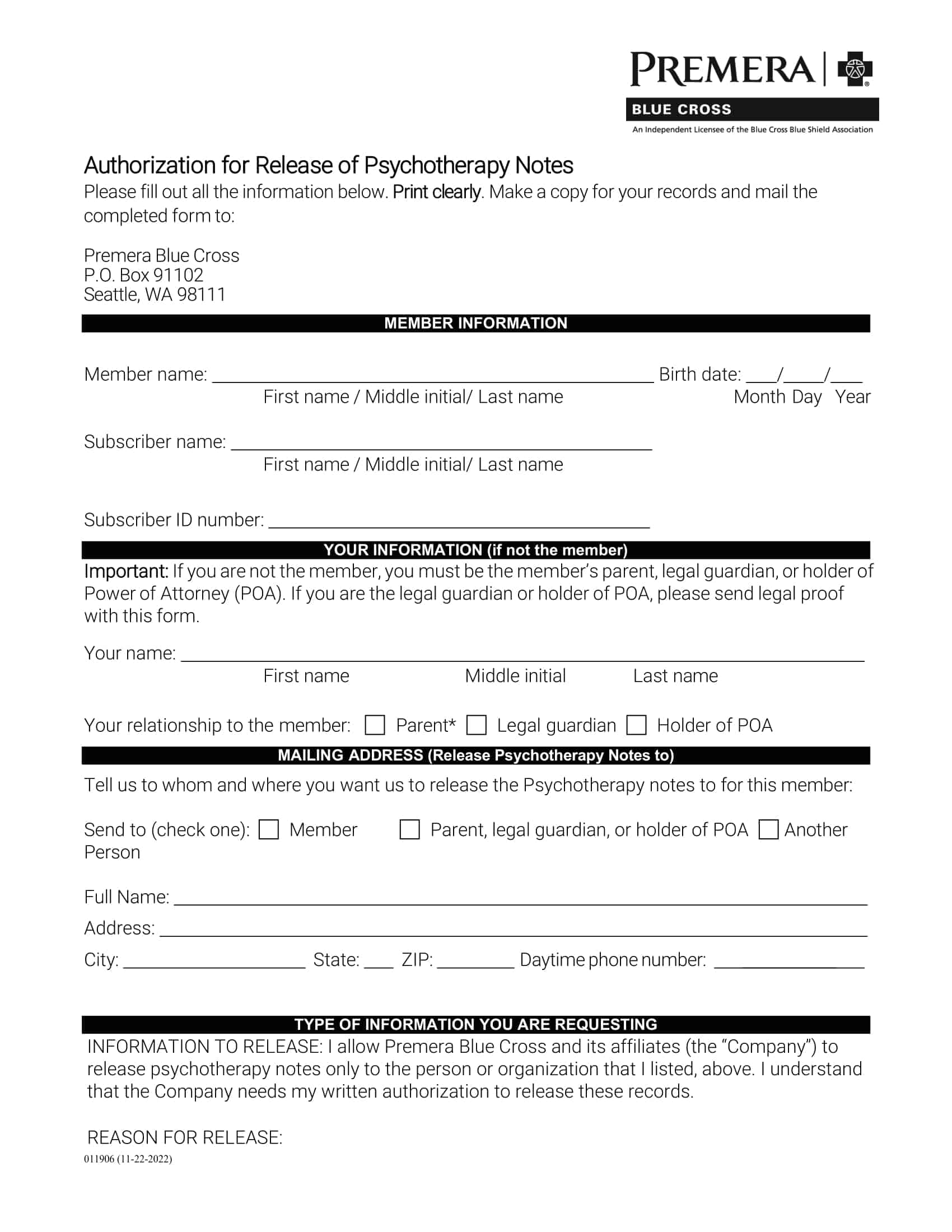
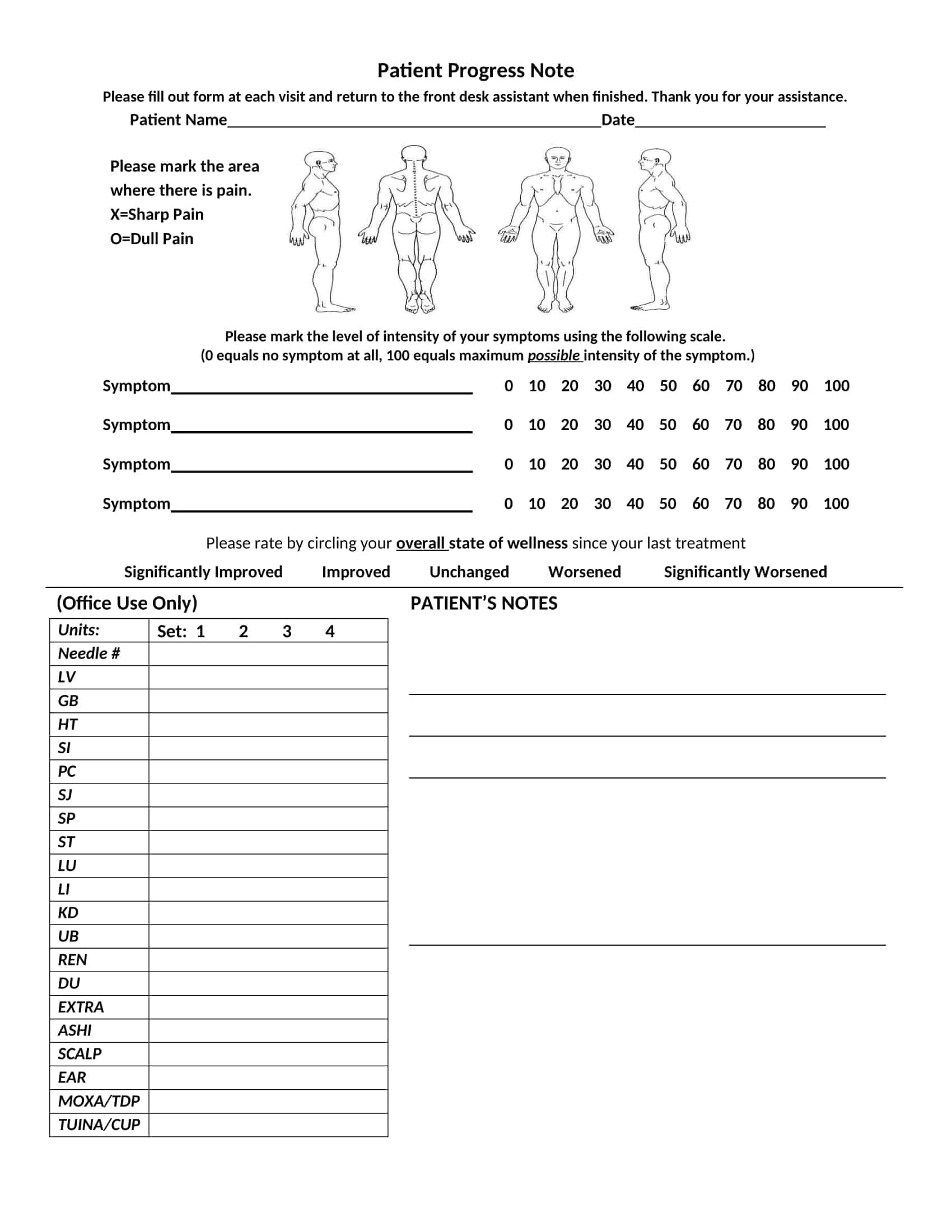
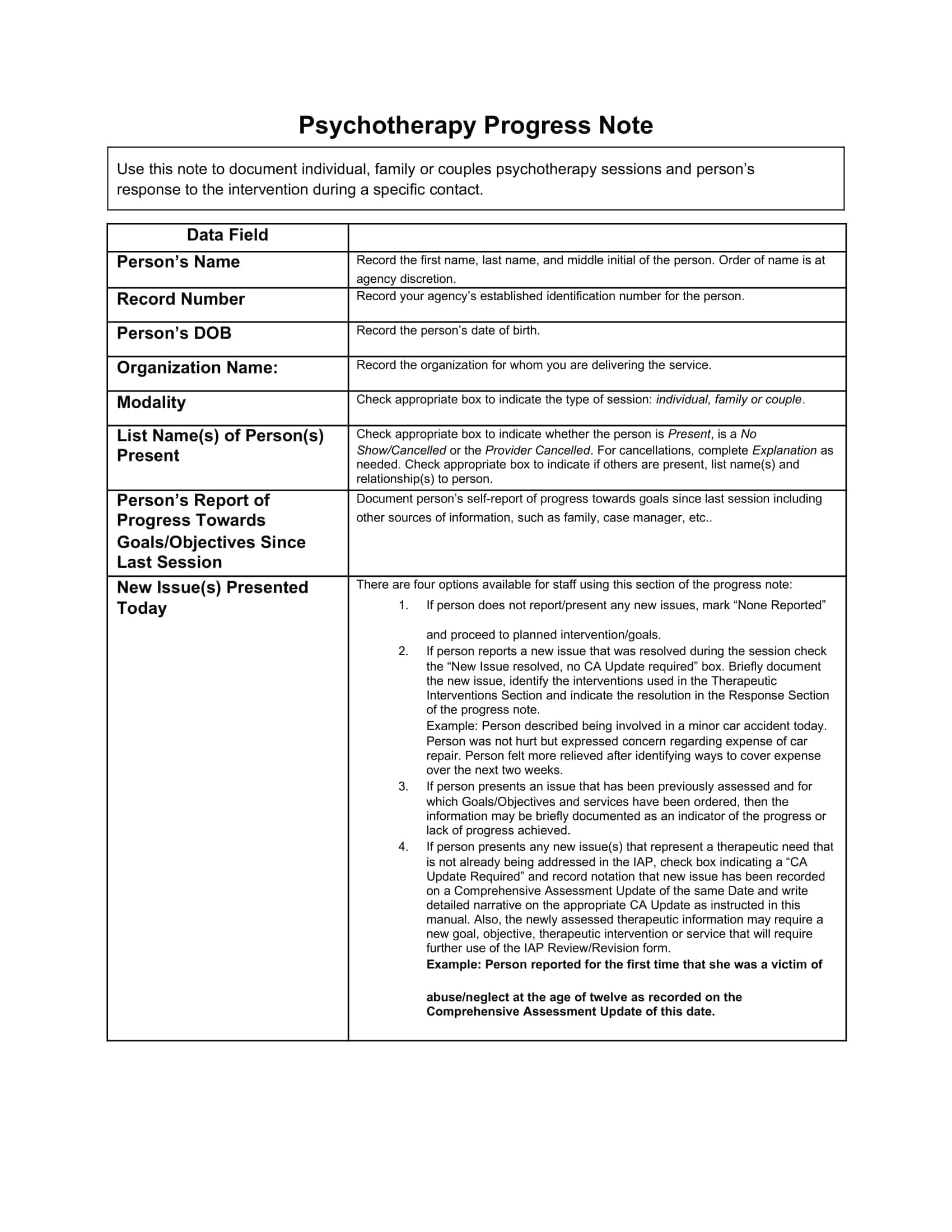
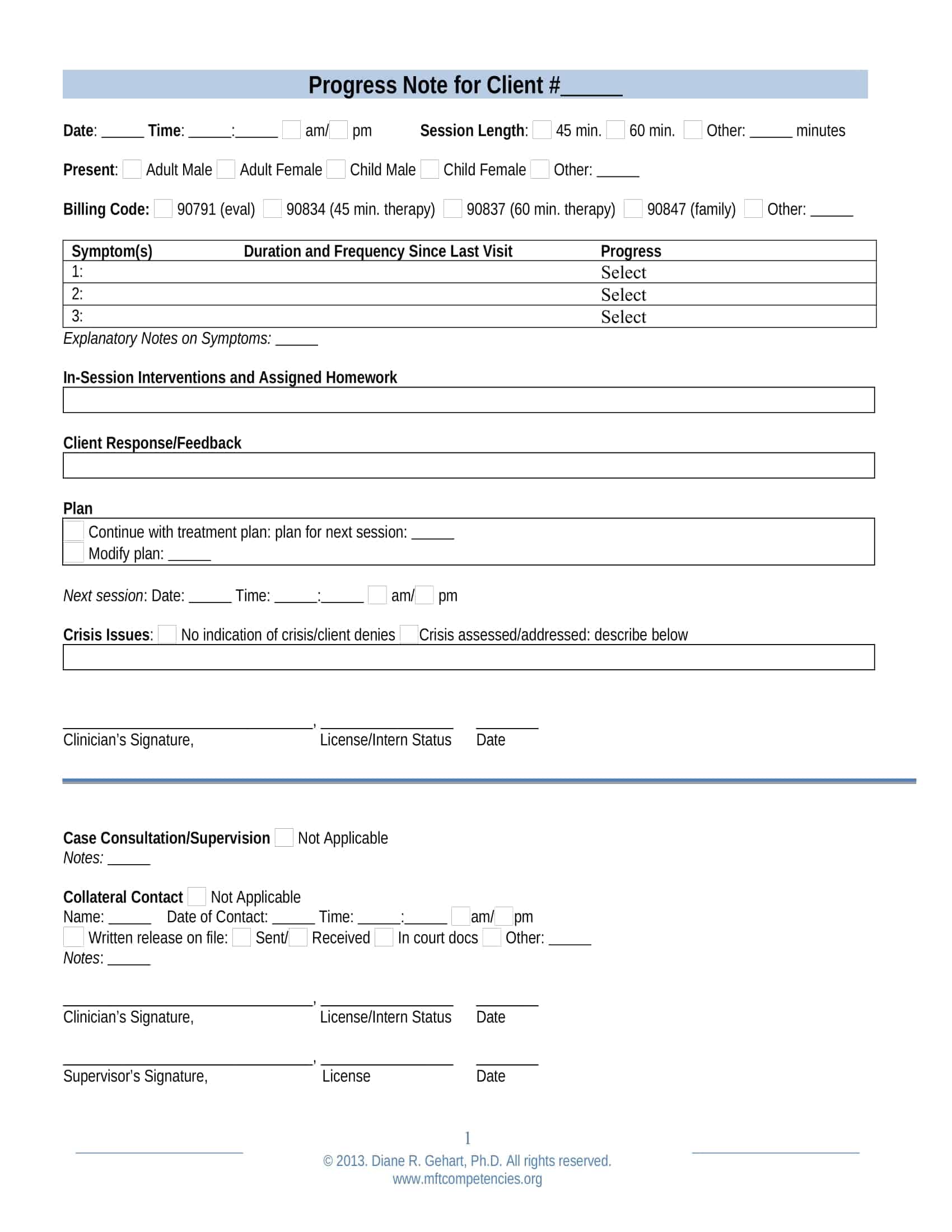
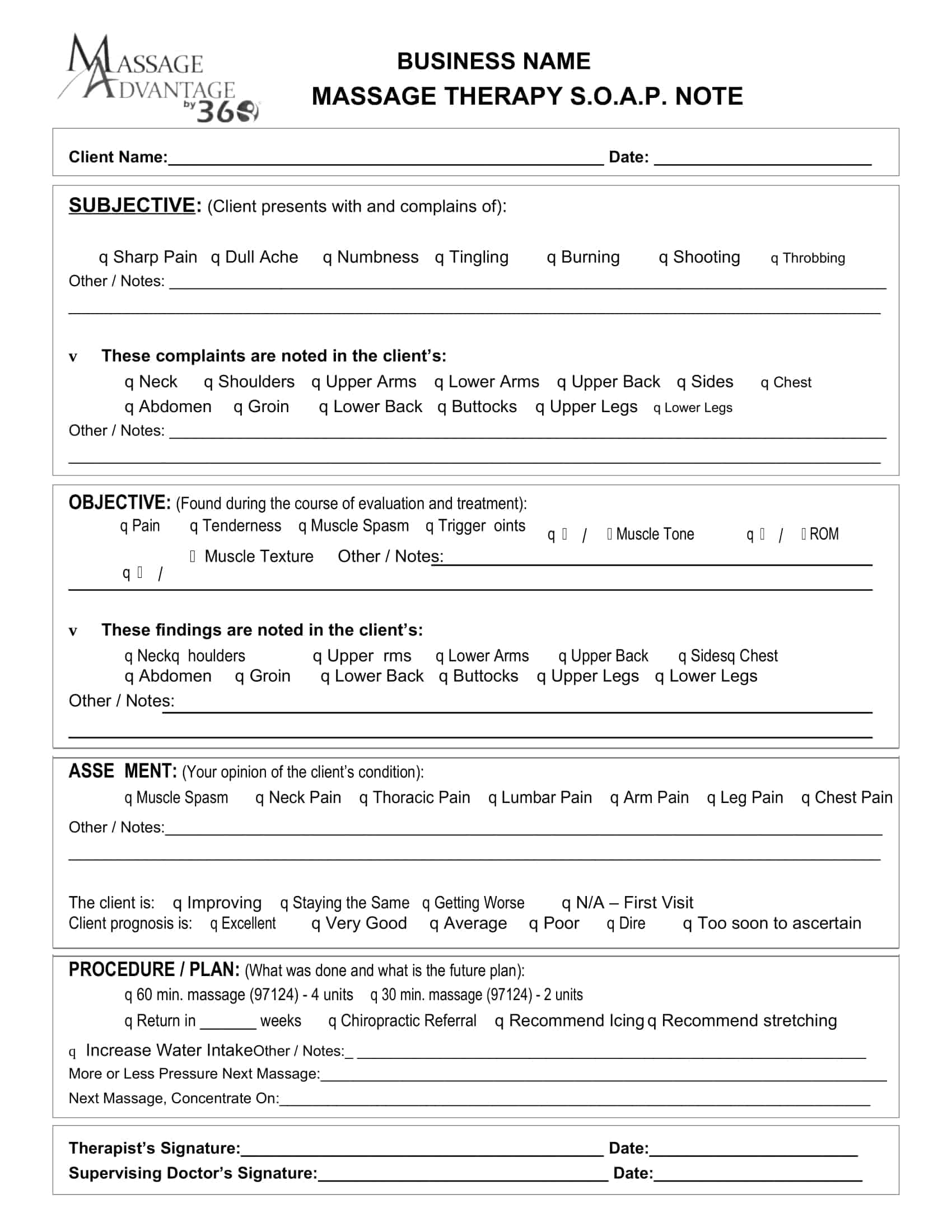
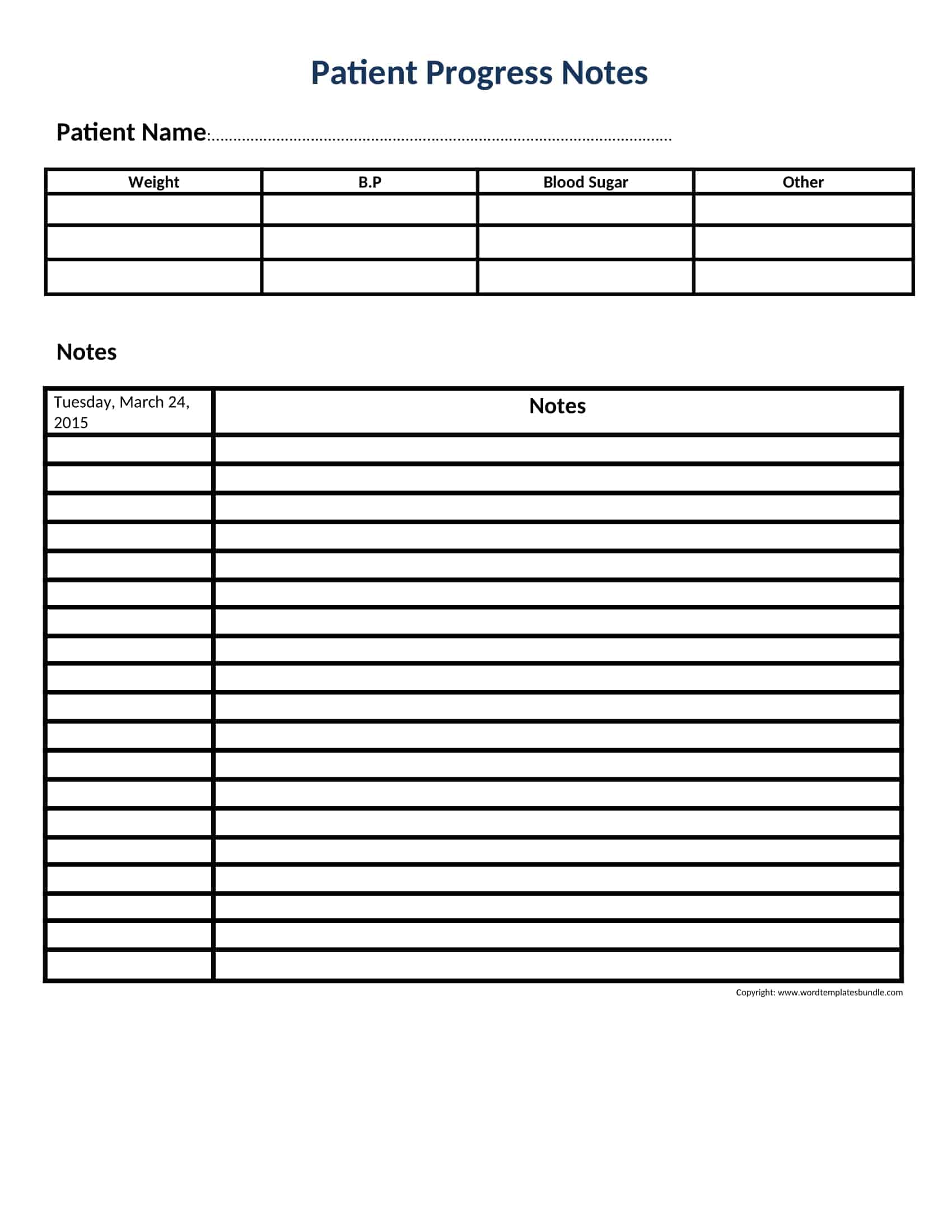
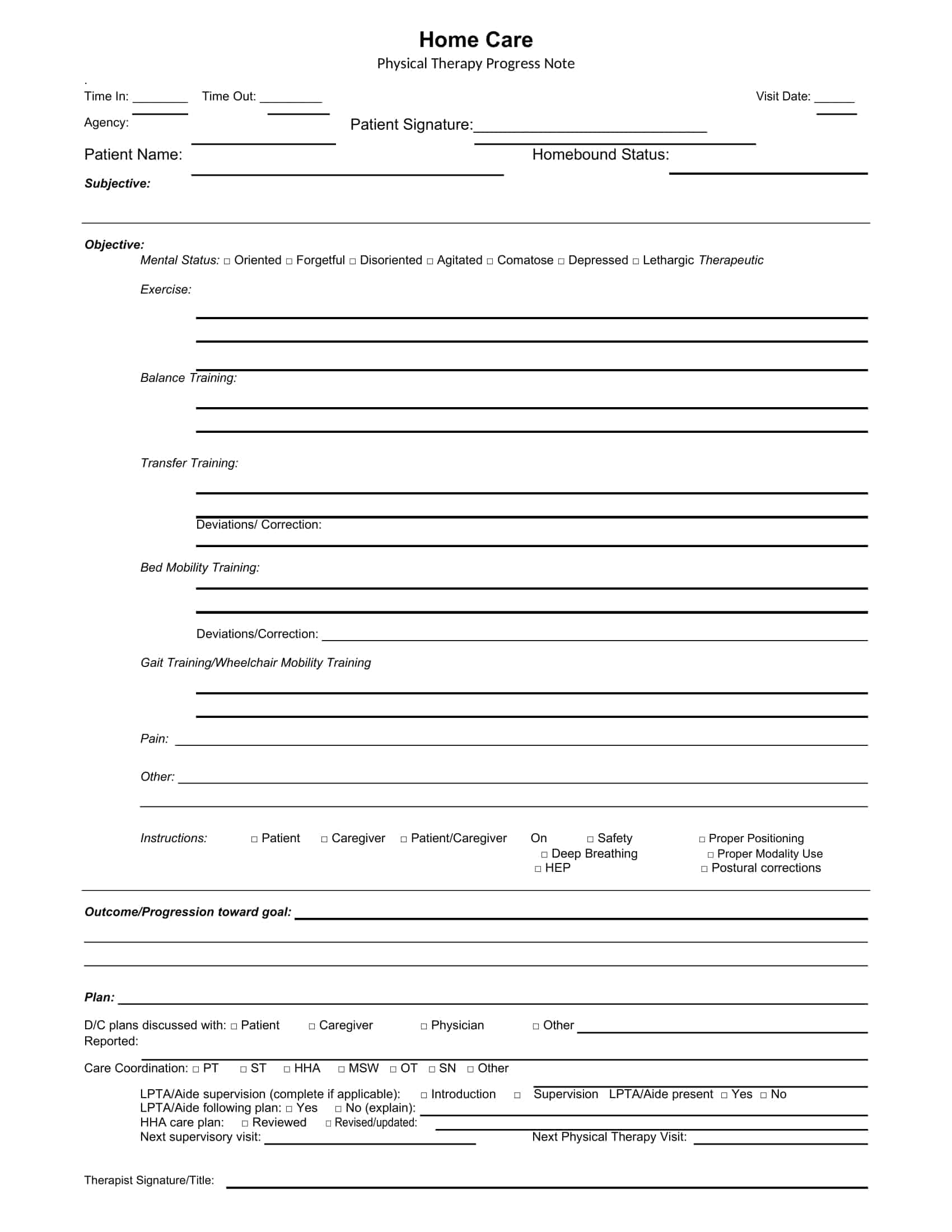
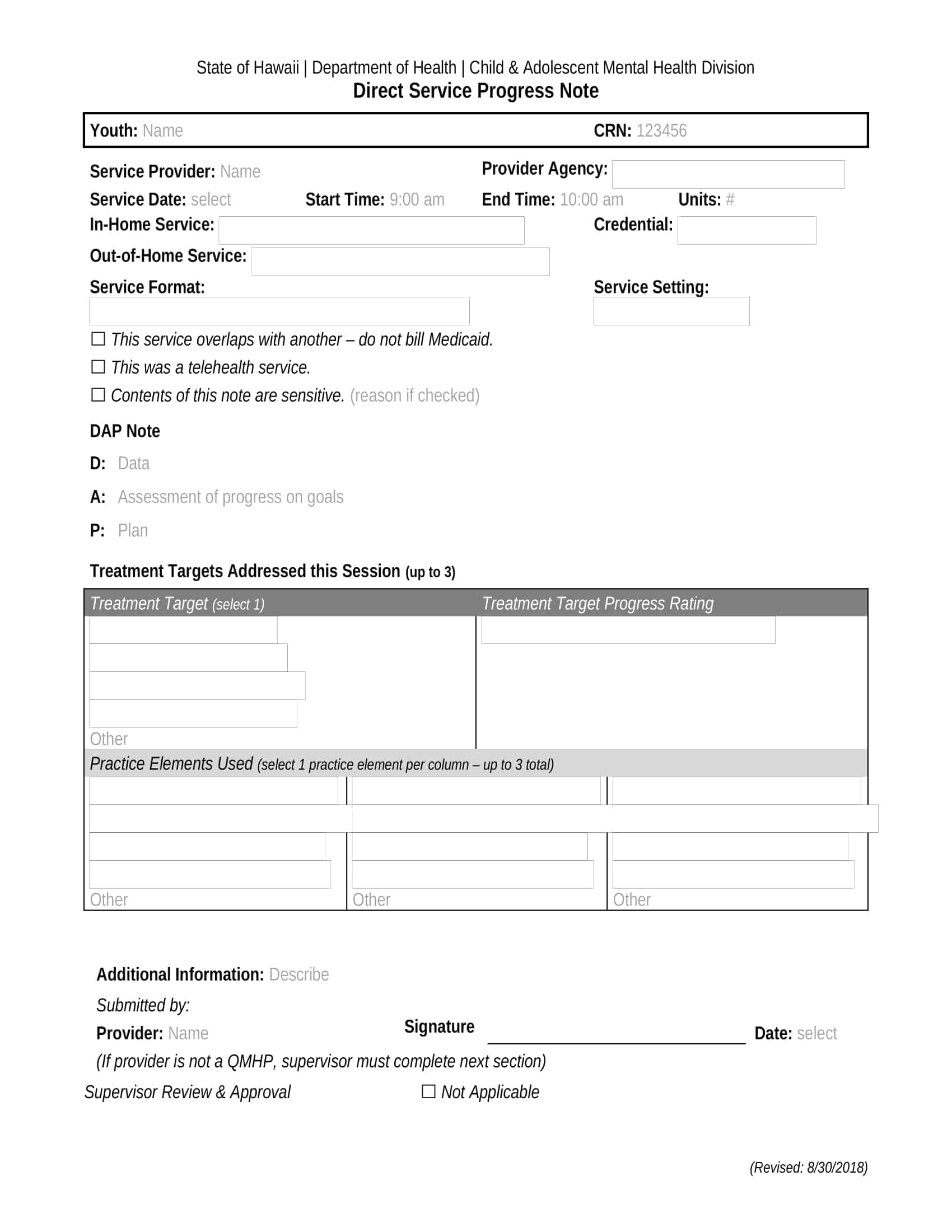
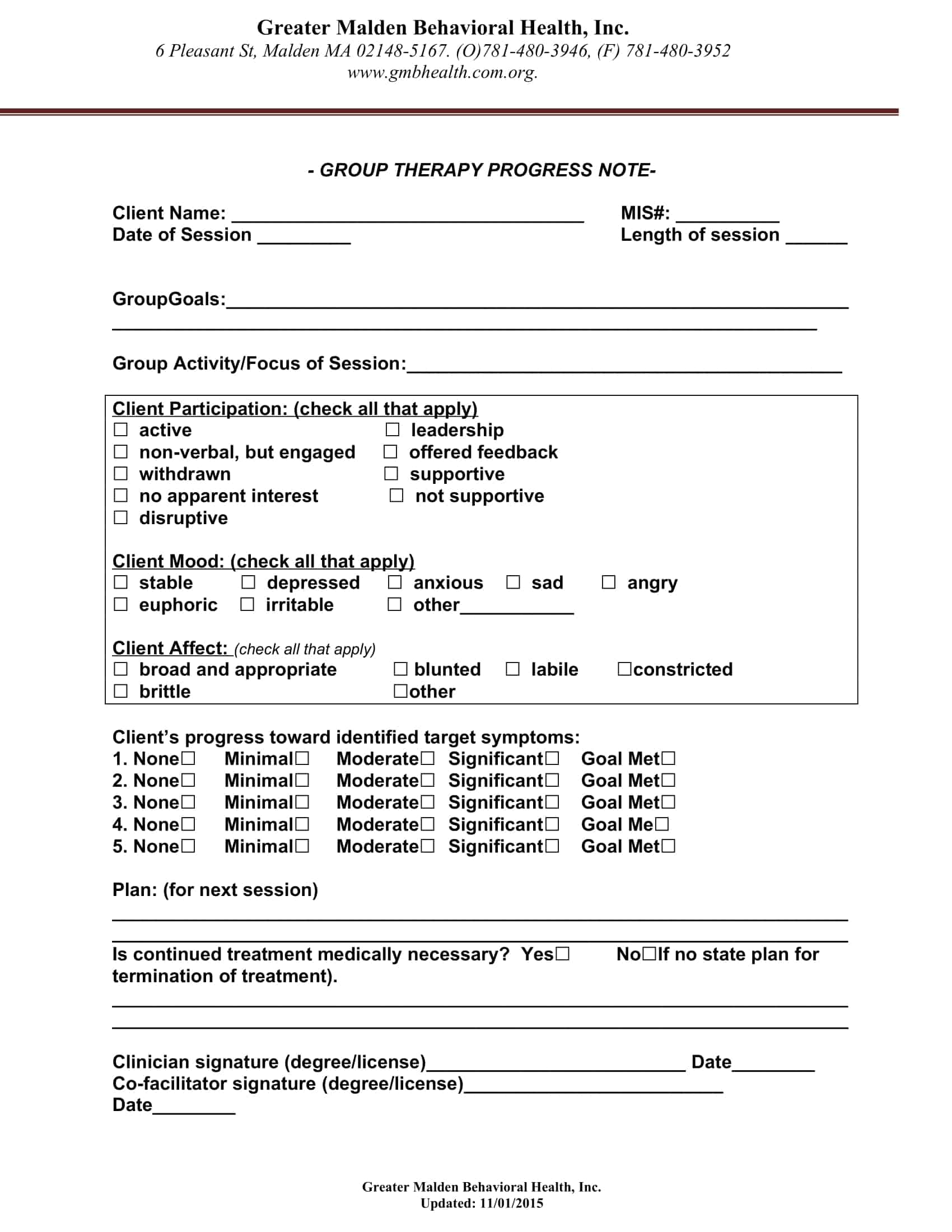
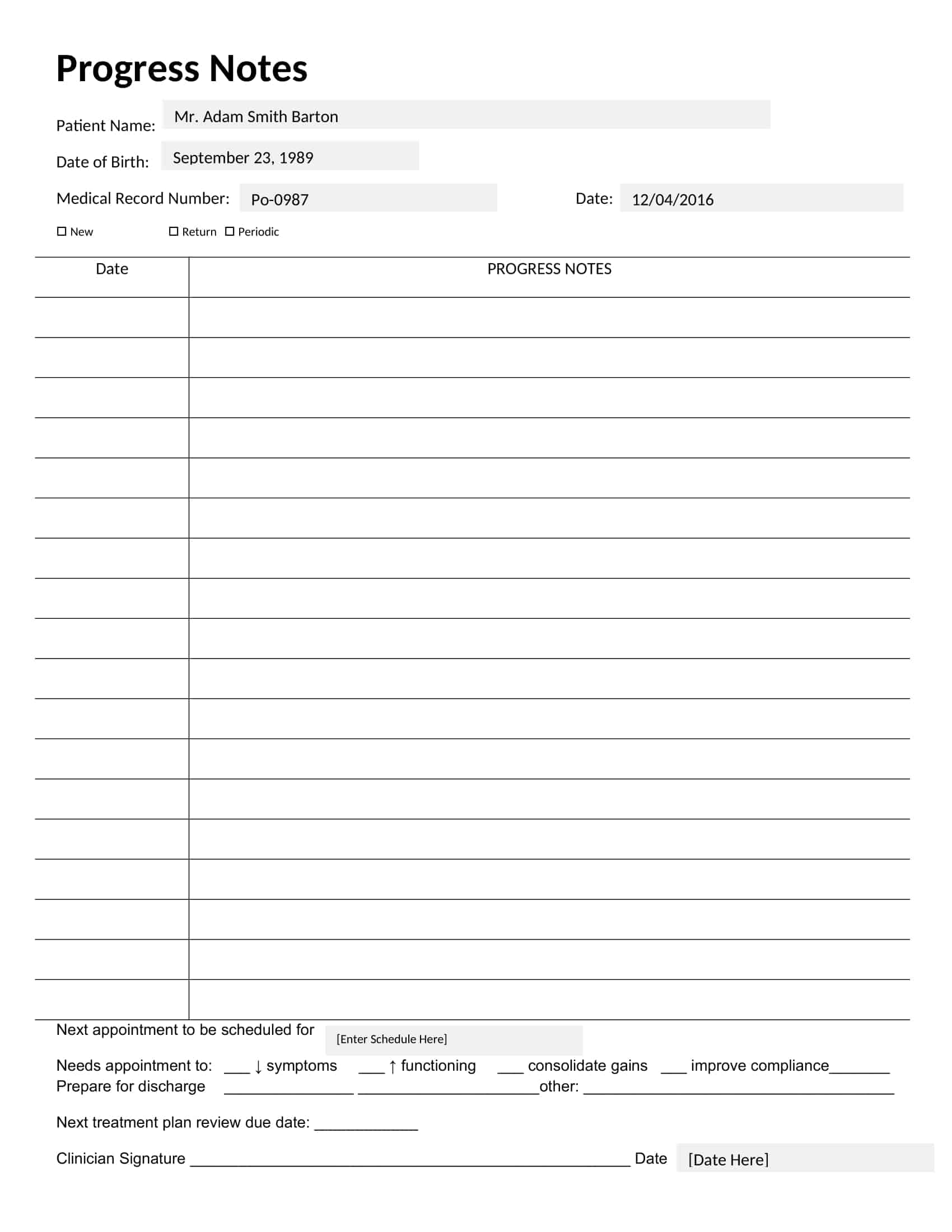
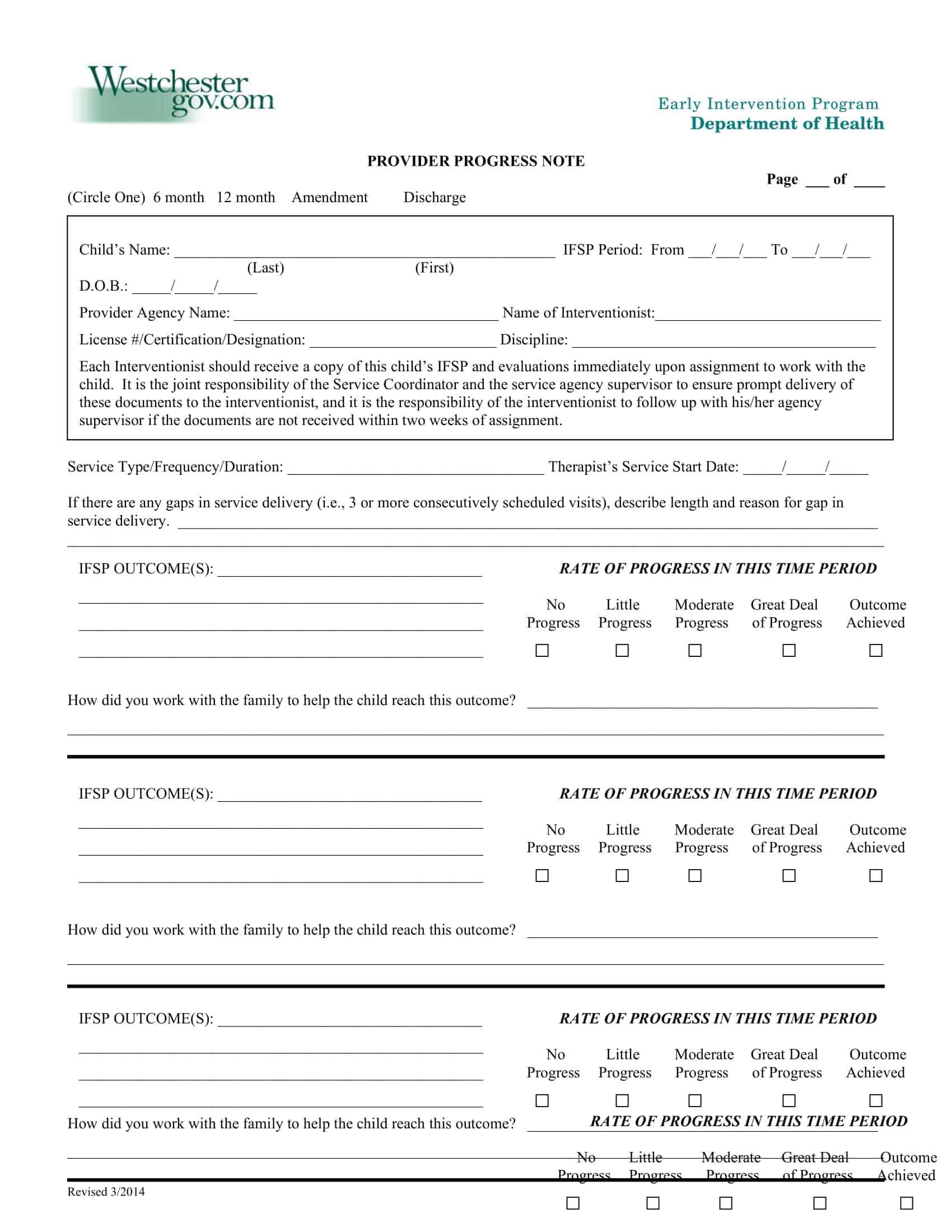
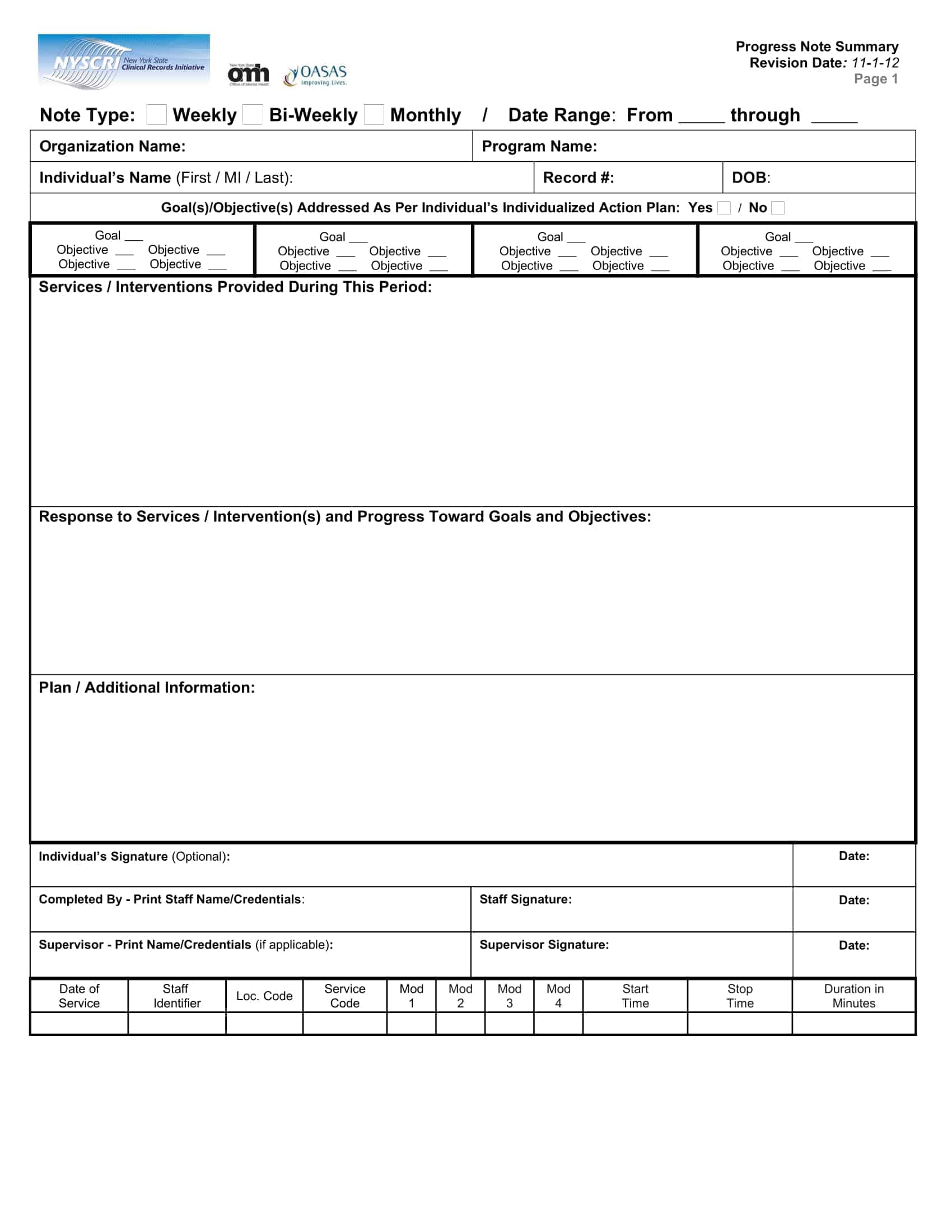
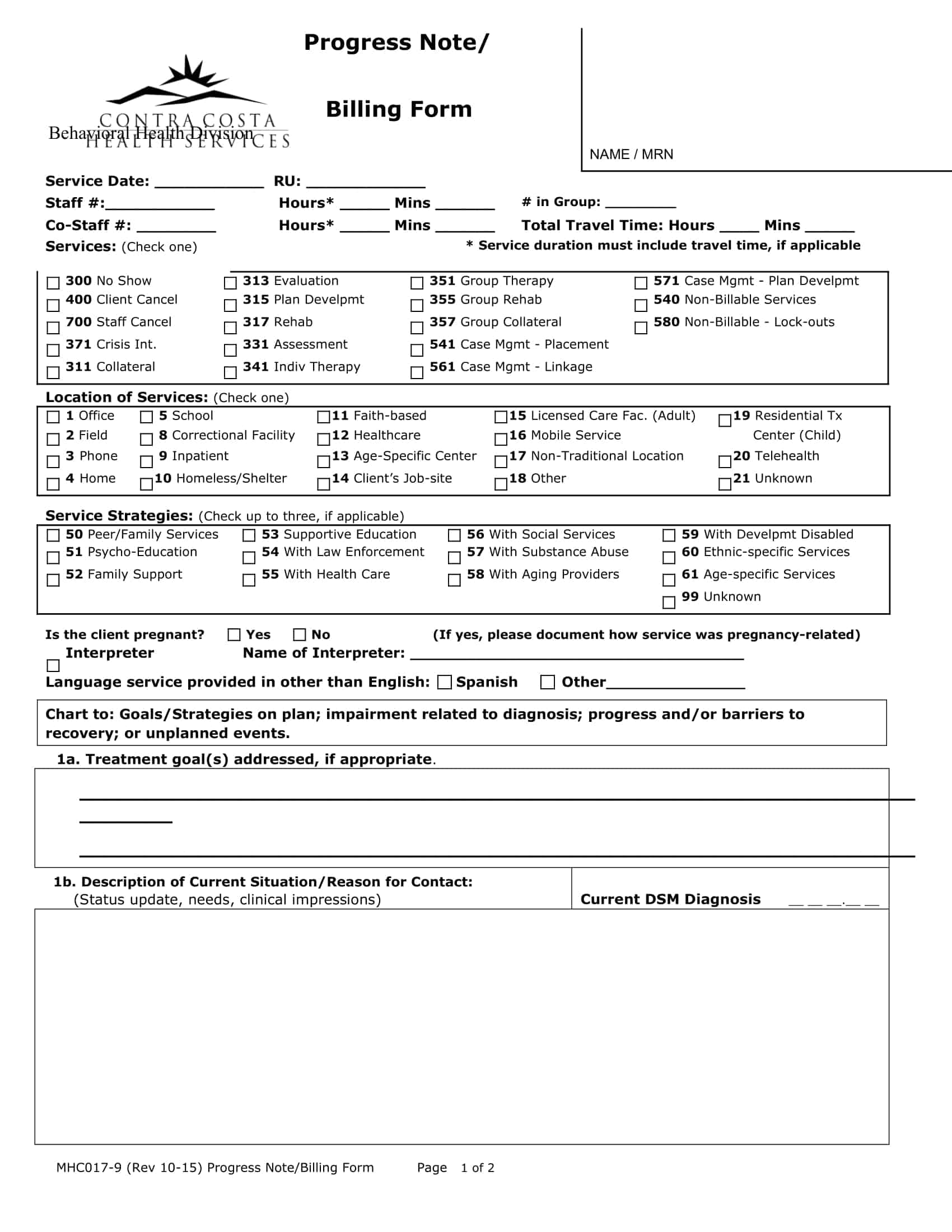
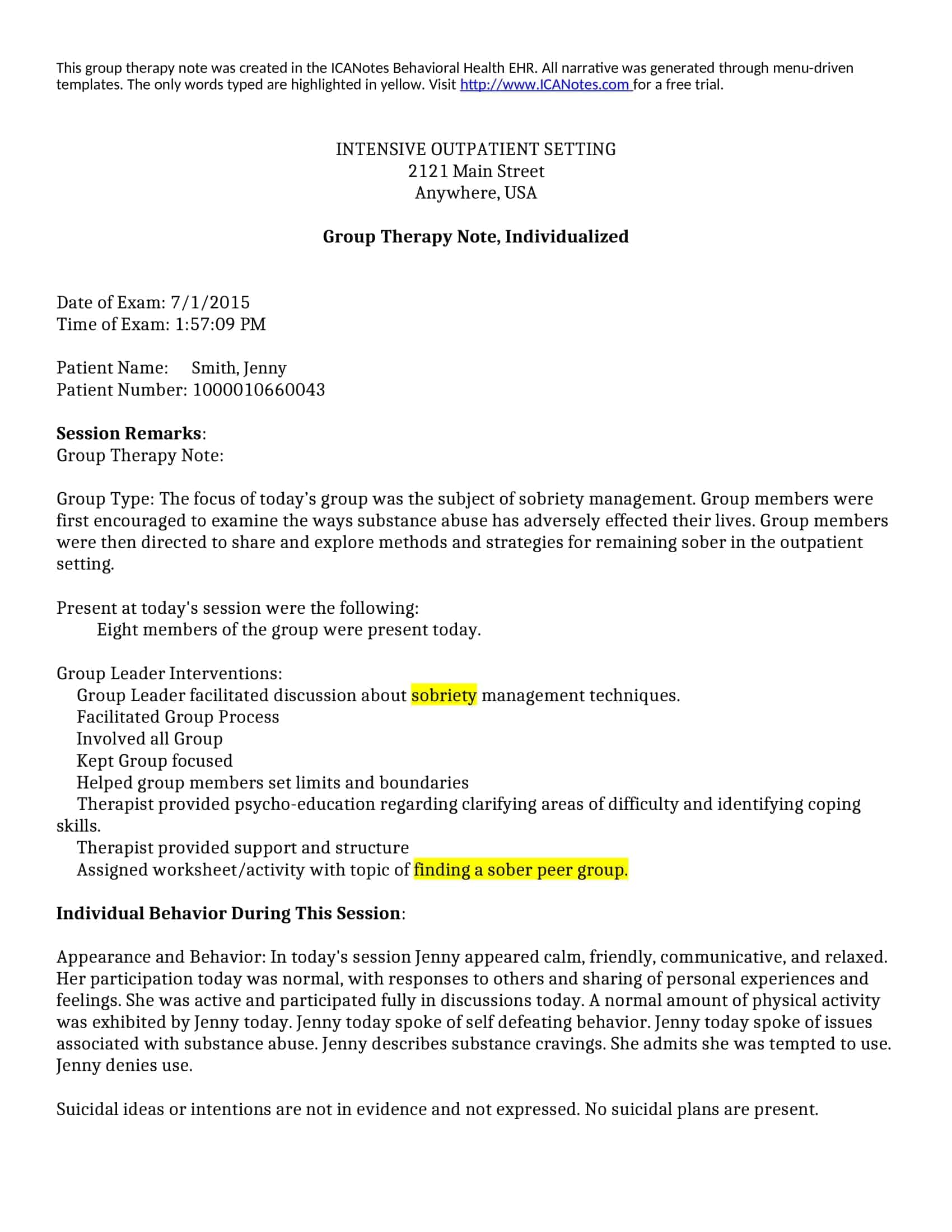
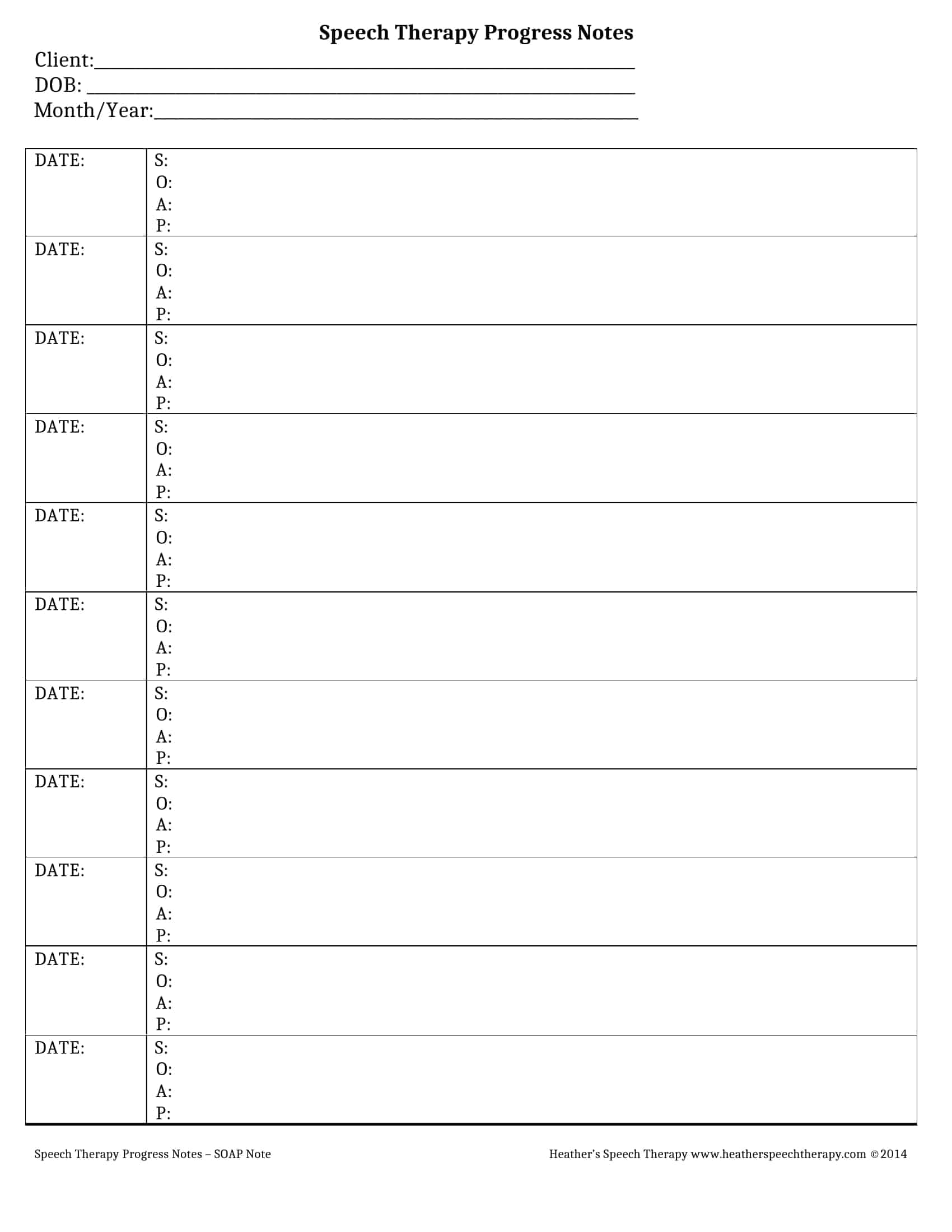
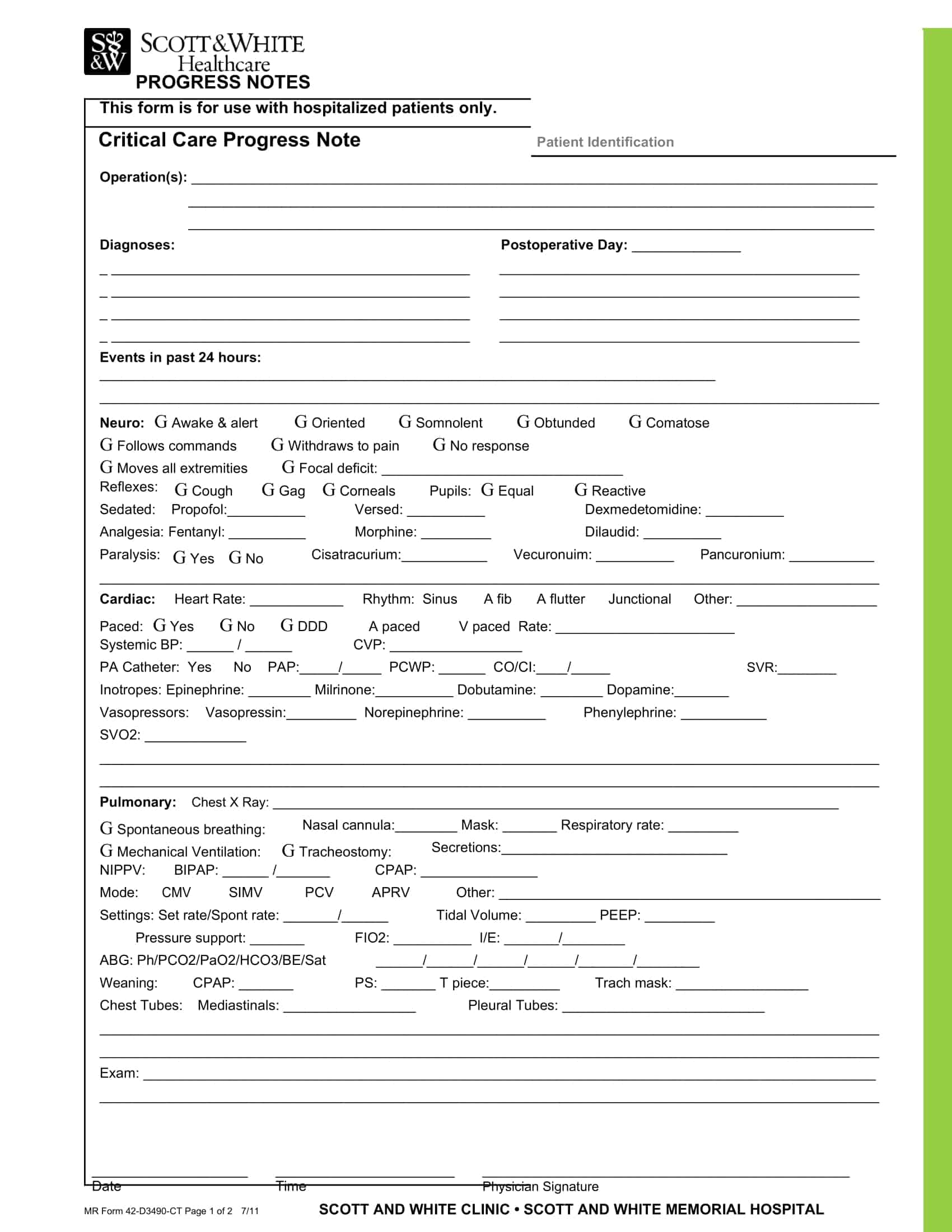
Therapy Notes Templates
Efficiently document and track therapy sessions with our comprehensive collection of Therapy Notes Templates. These customizable and printable templates provide a structured framework for recording important details, observations, and progress during therapy sessions. Whether you’re a therapist, counselor, or healthcare professional, our templates cover essential sections such as client information, session summaries, treatment plans, goals, interventions, and assessments.
By utilizing our Therapy Notes Templates, you can maintain accurate and organized records, track client progress over time, and ensure continuity of care. Our templates offer a convenient way to capture critical information, communicate with other healthcare providers, and adhere to professional standards and legal requirements. Streamline your therapy documentation process, enhance client care, and improve outcomes with our user-friendly templates. Download now and simplify the task of maintaining comprehensive and informative therapy notes.
Why Do Some Therapists Take Notes in Session?
Some therapists choose to take notes during a session for a variety of comprehensive reasons. Primarily, these notes serve as a way to document essential information about the client’s emotions, behaviors, thought patterns, and progress. By doing so, therapists can better remember details about each client and their unique needs, allowing them to provide more personalized and effective treatment.
Taking notes in-session also helps therapists monitor the therapeutic process by highlighting areas of improvement, identifying patterns, and evaluating the efficacy of various interventions. This ensures that therapists can adjust their approach accordingly to optimize the client’s progress and recovery.
Moreover, these notes are crucial for maintaining continuity of care, especially when working in a multidisciplinary team. Sharing relevant information about the client’s therapeutic journey with other healthcare professionals can improve overall treatment outcomes and help maintain a consistent approach.
In addition, therapy notes are often legally and ethically required to maintain accurate records of the therapeutic process. These records may be needed for insurance billing purposes, professional audits, or in the case of legal proceedings.
Finally, taking notes during a session can also provide therapists with the opportunity to model active listening and attentiveness. This can reassure clients that their concerns are being heard, validated, and addressed, thereby fostering a stronger therapeutic alliance.
Despite the potential benefits, it is essential for therapists to remain sensitive to the client’s comfort and to address any concerns they may have about note-taking during sessions. The therapist’s ultimate goal is to create an environment in which the client feels safe, supported, and able to openly discuss their thoughts and feelings.
Why is a counseling notes template essential for therapists?
Utilizing a counseling notes template offers numerous benefits for therapists, streamlining the process of documenting vital information during sessions.
Minimizes interruptions
When taking notes, therapists aim to minimize disruptions, allowing clients to freely express their thoughts and feelings. A counseling notes template is structured in such a way that therapists can quickly jot down key points, resulting in fewer distractions for the client.
User-friendly design
The preformatted nature of counseling notes templates simplifies their usage. Therapists can effortlessly fill in the required fields without needing to create a separate layout or structure for taking notes. This prearranged format makes the template highly convenient.
Protects client confidentiality
In most cases, therapists can directly input information into a digital counseling notes template, eliminating the need for physical copies. Paper-based records are more susceptible to unauthorized access, while digital files can be securely stored and protected with passwords or encryption. This approach ensures that sensitive client information remains confidential and accessible only to authorized individuals.
Difference Between Progress & Psychotherapy Notes
Progress notes and psychotherapy notes (also known as process notes) are two distinct types of therapy notes used by mental health professionals. While both document the therapy process, they have different purposes, levels of detail, and confidentiality protections. Here are the main differences between progress notes and psychotherapy notes:
Purpose:
Progress notes serve as a concise, objective summary of a therapy session, focusing on the key points and interventions used during the session. They help track the client’s progress over time, inform future sessions, and provide a record of treatment for other healthcare providers or third-party payers if needed. Progress notes are part of the client’s official record.
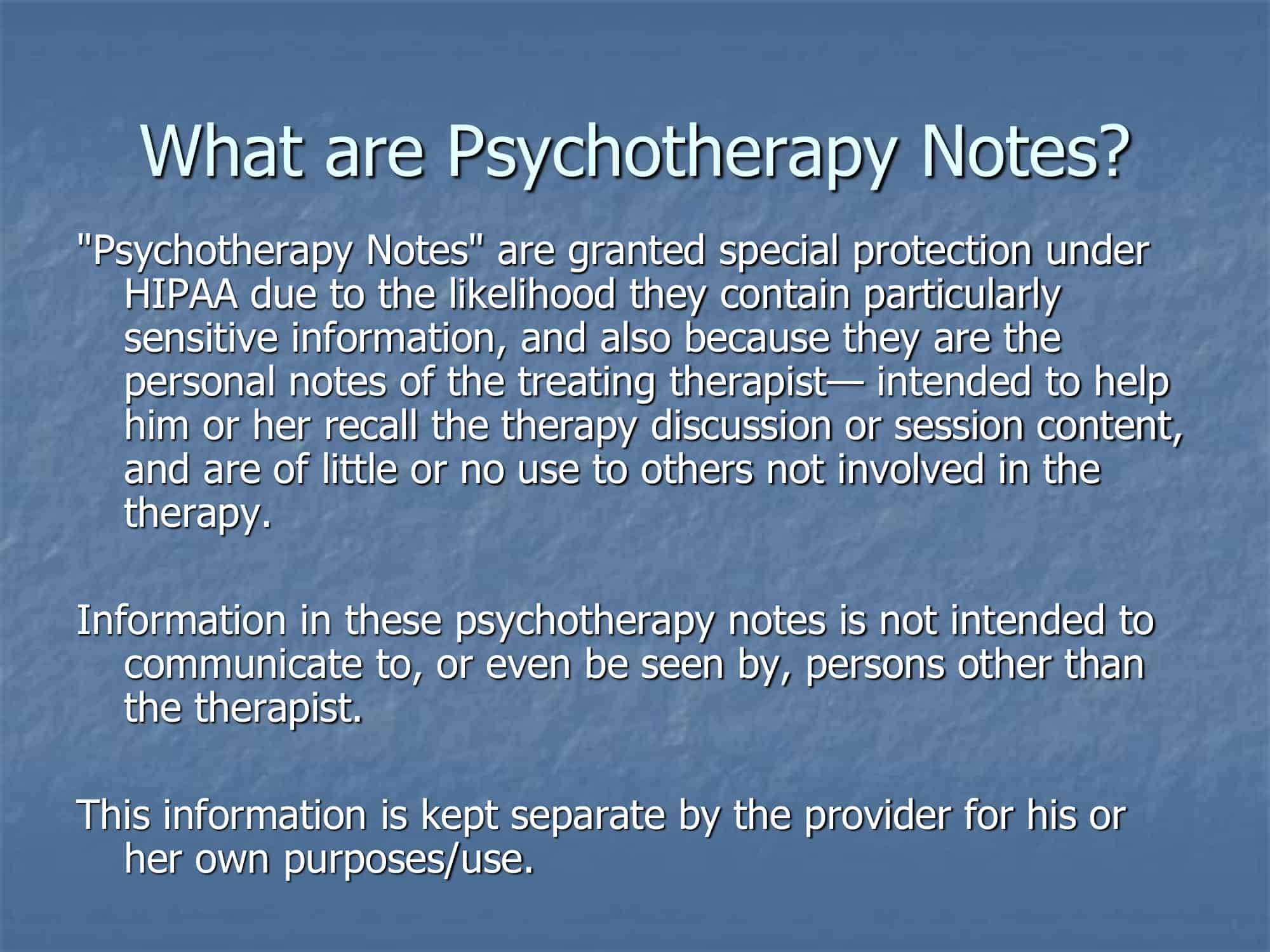
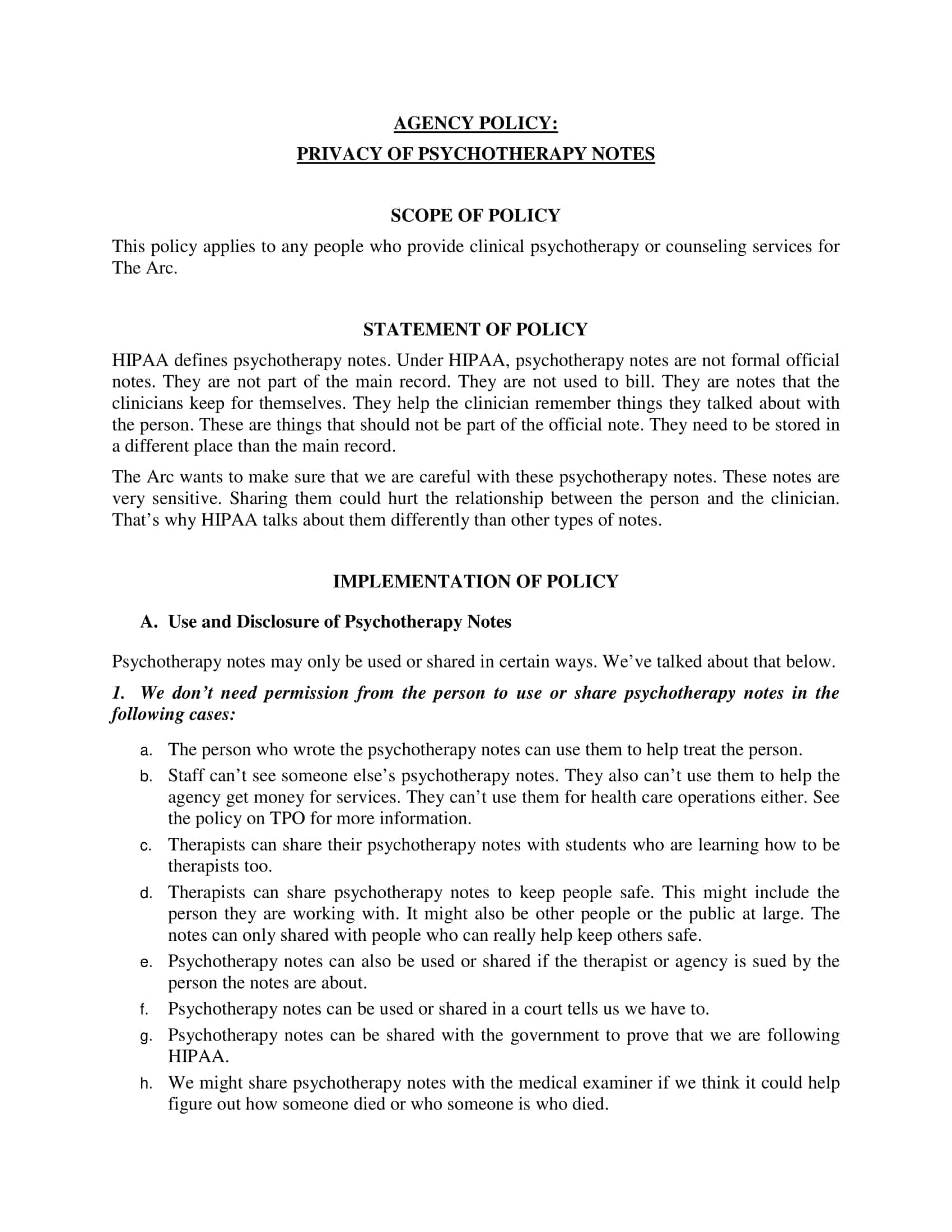
Psychotherapy notes, on the other hand, provide a more detailed and subjective account of the therapist’s thoughts, impressions, and interpretations of the therapy session. They often include the therapist’s personal observations and reflections on the therapeutic process. Psychotherapy notes are intended primarily for the therapist’s use and are kept separate from the client’s official record.
Content:
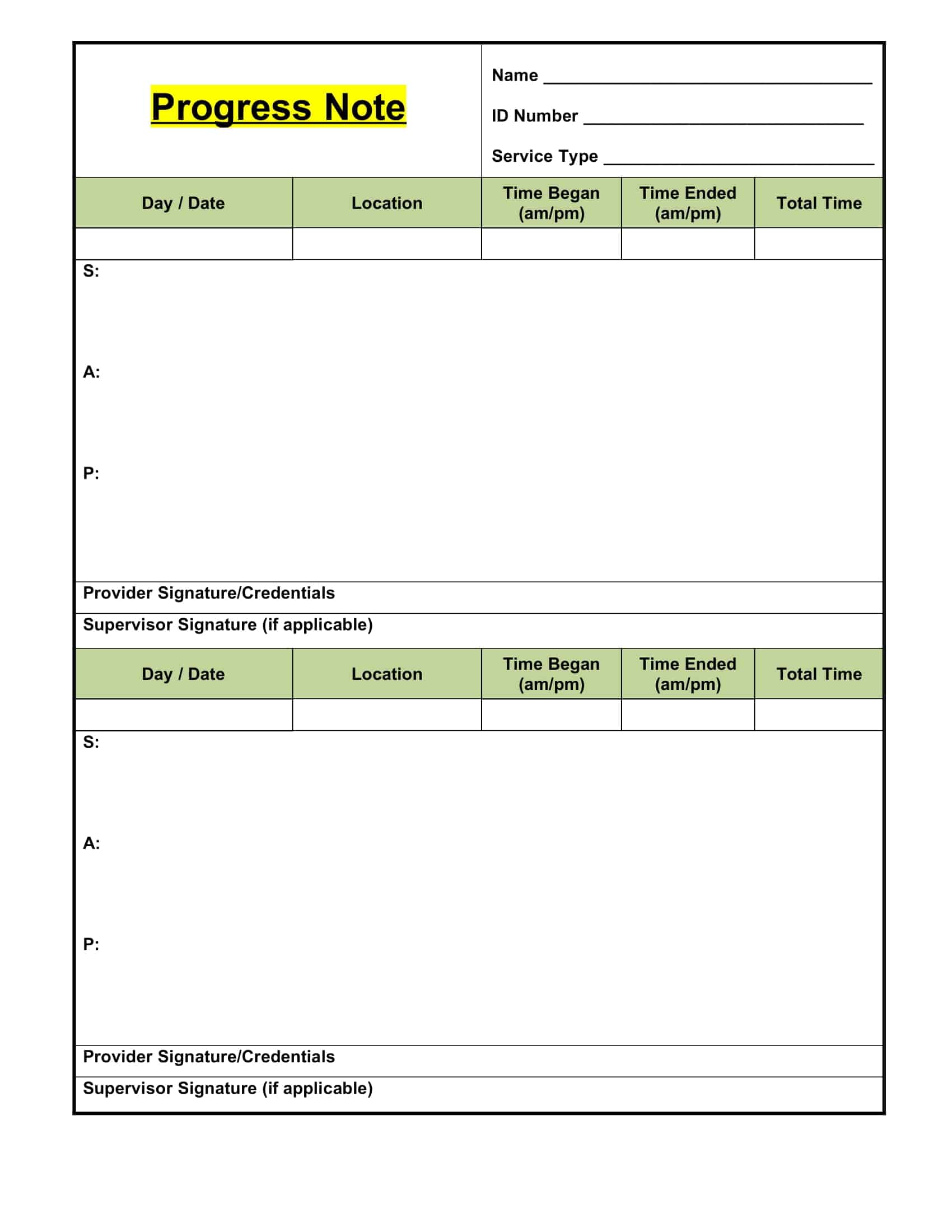
Progress notes typically follow a structured format, such as SOAP (Subjective, Objective, Assessment, Plan) or DAP (Data, Assessment, Plan), which includes information about the client’s presenting issues, the interventions used during the session, the client’s response to those interventions, and any significant events or changes. They are brief and factual, focusing on observable behaviors, interventions, and outcomes.
Psychotherapy notes, in contrast, are less structured and more comprehensive. They may include the therapist’s observations, hypotheses, and insights about the client’s thoughts, feelings, and behaviors, as well as any countertransference or reactions the therapist may have experienced during the session. Psychotherapy notes can be more in-depth and subjective compared to progress notes.
Confidentiality:
Progress notes are part of the client’s official record and may be accessed by other healthcare professionals, third-party payers, or legal entities with the client’s consent or as required by law. As a result, progress notes must adhere to strict confidentiality guidelines and should not include sensitive or private information that is not directly relevant to the client’s treatment.
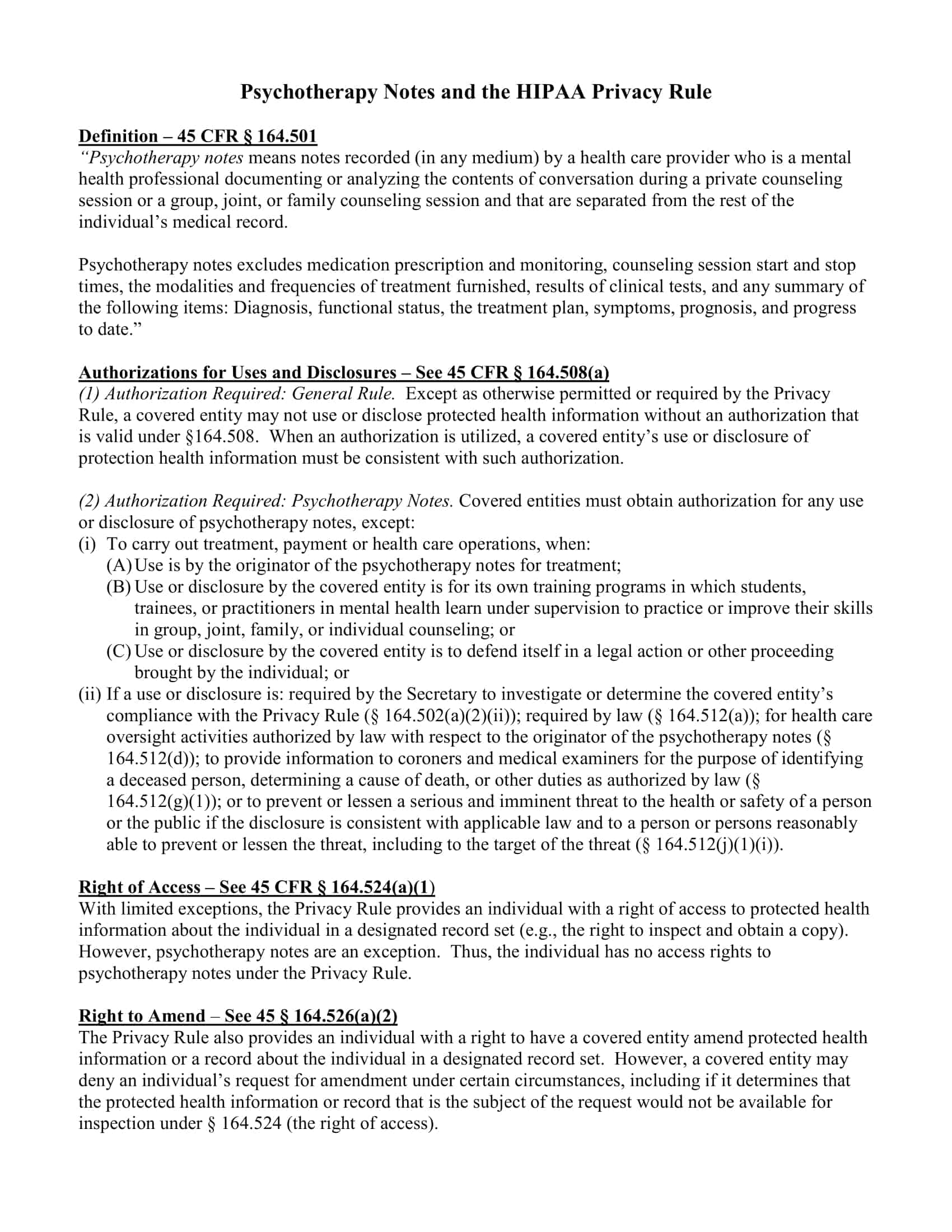
Psychotherapy notes, on the other hand, are kept separate from the client’s official record and are granted a higher level of confidentiality protection under the Health Insurance Portability and Accountability Act (HIPAA). They are generally not disclosed to third parties or shared with other healthcare providers without the client’s explicit consent. However, psychotherapy notes may still be subject to disclosure in certain legal circumstances, such as court orders or subpoenas.
In summary, progress notes are objective, concise summaries of therapy sessions used to track progress and inform future treatment, while psychotherapy notes are more detailed, subjective accounts of the therapist’s observations and reflections on the therapy process. Progress notes are part of the client’s official record and have less confidentiality protection, whereas psychotherapy notes are kept separate and enjoy a higher level of confidentiality protection.
What should be included in therapy notes?
Therapy notes are essential for therapists to effectively recall sessions with clients, ensuring proper follow-up and successful treatment. These records also play a significant role in insurance reimbursement. To create effective therapy notes, the following components should be included:
Client demographics
Capture essential demographic information to prevent confusion between clients. Include:
- Client name
- Age
- Gender
- Ethnicity
- Employment status
- Marital status
- Physical address
This information provides valuable context when creating individualized treatment plans.
Client diagnosis
Include the client’s diagnosis, along with the relevant ICD code (International Classification of Diseases) for billing and insurance purposes.
Client’s presenting issue
Document the client’s issue in their own words. This information will be crucial when reviewing the notes to develop an effective mental health treatment plan.
Safety considerations
Record any safety concerns related to the client, their immediate family, or yourself as the therapist. This may involve potential harm, suicidal ideation, or other threats.
Medications prescribed
Document the client’s current medications, including:
- Medication type
- Dosage
- Start and end dates
- Purpose
- Side effects experienced
Understanding the client’s medications can help assess potential impacts on their mental health.
Symptom history
Record the client’s symptom history, including how these symptoms have affected their health, relationships, and work. Document any previous treatments and their outcomes.
Current mental status
Describe the client’s mental status, observing their mood, behavior, and appearance. Note any unusual observations that may be relevant to their treatment.
Interventions utilized
Document the therapeutic interventions implemented and the primary issues addressed during the session. For subsequent sessions, note whether the client followed previous instructions and their willingness to comply or resist.
Treatment plans and goals
Outline the treatment plan, specifying the recommended therapy approach, such as:
- Behavior therapy
- Humanistic therapy
- Integrative therapy
- Cognitive therapy
- Psychoanalysis therapy
Explain how the chosen intervention will aid the client’s progress, and list any actions or assignments for them to complete.
Progress notes
For each session, document any observable progress, noting whether the client’s symptoms are improving or worsening. If no improvement is observed, identify the reasons and consider alternative approaches or therapies. Referring to progress note examples can offer further insights.
How to Write a Therapy Note: A Step-by-Step Guide
Writing effective therapy notes is crucial for tracking client progress, maintaining continuity of care, and ensuring legal and ethical compliance. Follow this step-by-step guide to create comprehensive therapy notes:
Prepare before the session:
Before meeting with your client, have a template or format ready for your therapy notes. This will help you stay organized and focused during the session, as you’ll already have a structure to follow.
Begin with the basic client information:
Start your therapy note by recording the client’s identifying information, including their name, date of birth, and contact details. Make sure to also include the date and duration of the session.
Document the client’s presenting issue:
In this section, describe the client’s reason for seeking therapy. Be sure to capture their concerns and symptoms in their own words, providing an accurate representation of their situation.
Record your observations of the client’s mental status:
Describe the client’s mental state during the session by noting their mood, affect, behavior, thought patterns, and appearance. Pay attention to any changes or significant observations that may be relevant to their treatment.
Summarize the session’s content:
Provide an overview of the session, outlining the topics discussed and the therapeutic interventions used. Be concise yet thorough, capturing the essence of the conversation and the client’s responses to your interventions.
Document client progress and response to treatment:
Describe any changes in the client’s symptoms or behaviors, noting improvements, setbacks, or stagnation. Evaluate the effectiveness of the interventions used and adjust your treatment plan accordingly if needed.
Note any safety concerns or risk factors:
If applicable, document any safety concerns or risk factors related to the client, their family, or yourself as the therapist. This may include suicidal ideation, self-harm, or potential harm to others.
Outline the treatment plan and goals:
Detail the client’s short-term and long-term therapeutic goals, as well as the specific treatment strategies and interventions you plan to use. Ensure these goals are specific, measurable, achievable, relevant, and time-bound (SMART).
Assign homework or tasks for the client:
If appropriate, assign homework or tasks for the client to complete between sessions. This can help reinforce the therapeutic work done in-session and promote continued progress outside of therapy.
Plan for the next session:
Briefly outline any topics or interventions you plan to address in the next session, ensuring continuity and a clear direction for future meetings.
Review and revise your notes:
After completing your therapy notes, take some time to review and revise them for clarity, accuracy, and comprehensiveness. Ensure you’ve captured all relevant information and that your notes are well-organized and easy to understand.
Store your therapy notes securely:
Finally, ensure your therapy notes are stored securely, whether in a locked cabinet for paper-based notes or password-protected electronic files. This is crucial for maintaining client confidentiality and adhering to legal and ethical guidelines.
Types of Therapy Notes
Therapy notes, also known as progress notes or case notes, are documents that mental health professionals create to record information about their clients’ sessions. These notes serve as a record of the therapeutic process and are used for various purposes, including tracking progress, planning future sessions, and coordinating care with other professionals. There are several types of therapy notes, and each has its unique purpose and format. Some common types include:
Process Notes:
Process notes, sometimes called psychotherapy notes, provide a detailed account of the content and dynamics of a therapy session. They may include the therapist’s observations, interpretations, and reflections on the client’s thoughts, feelings, and behaviors. Process notes are often more detailed and subjective than other types of therapy notes, and they are typically kept separate from the main client record to maintain privacy.
Progress Notes:
Progress notes are a concise, objective summary of each therapy session. They typically include information about the client’s presenting issues, interventions used during the session, the client’s response to those interventions, and any significant events or changes. Progress notes follow a specific format, such as SOAP (Subjective, Objective, Assessment, Plan) or DAP (Data, Assessment, Plan), and are part of the client’s official record.
Treatment Plans:
Treatment plans outline the goals and objectives of therapy, the interventions and techniques that will be used to achieve these goals, and a timeline for progress. Treatment plans are created collaboratively between the therapist and client and are regularly reviewed and updated as needed. They serve as a roadmap for therapy and help to ensure that both parties have a clear understanding of the therapeutic process.
Intake Notes:
Intake notes are created during the initial assessment session and provide an overview of the client’s presenting issues, relevant history, and any other pertinent information. Intake notes typically include demographic information, a summary of the client’s concerns and goals, and an initial treatment plan. These notes serve as a foundation for future therapy sessions and help the therapist to tailor their approach to the client’s needs.
Termination Notes:
Termination notes document the conclusion of therapy, summarizing the client’s progress, the reasons for ending therapy, and any recommendations for future care. These notes may also include a summary of the therapeutic relationship, any unresolved issues, and the client’s overall satisfaction with the therapy process.
Consultation Notes:
Consultation notes are created when a therapist consults with another professional (e.g., psychiatrist, social worker, or another therapist) about a client’s case. These notes summarize the consultation, including any recommendations, insights, or additional resources provided by the consulting professional. Consultation notes help to coordinate care and ensure that the client receives comprehensive support.
FAQs
Here are some frequently asked questions (FAQs) about therapy notes, along with their answers:
Are therapy notes confidential?
Yes, therapy notes are generally considered confidential and are protected under various privacy laws and professional ethical guidelines, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States. However, there are certain situations in which confidentiality may be breached, such as when the client poses a risk to themselves or others, when a court order requires disclosure, or when the client consents to share the information with other healthcare providers or third-party payers.
What is the difference between progress notes and psychotherapy notes?
Progress notes are concise, objective summaries of therapy sessions, focusing on the key points and interventions used during the session. They are part of the client’s official record and may be accessed by other healthcare professionals or third-party payers with the client’s consent or as required by law. Psychotherapy notes, on the other hand, are more detailed and subjective accounts of the therapist’s thoughts, impressions, and interpretations of the therapy session. They are kept separate from the client’s official record and enjoy a higher level of confidentiality protection.
How long should therapy notes be retained?
The retention period for therapy notes varies depending on the jurisdiction, professional guidelines, and specific situations. In general, therapists are advised to retain client records, including therapy notes, for a minimum of 7 years after the last date of service. However, some states or professional organizations may require a longer retention period, and records related to minors may need to be retained until the client reaches a certain age (e.g., 18 or 21 years old). It is essential to be familiar with the relevant laws and guidelines in your jurisdiction.
Can clients access their therapy notes?
Clients generally have the right to access their own therapy records, including progress notes, as part of their right to privacy and informed consent. However, there may be exceptions or limitations in certain situations, such as when the therapist believes that disclosure may cause harm to the client or others. Psychotherapy notes, which are kept separate from the client’s official record, have a higher level of confidentiality protection and are generally not disclosed to clients or other parties without the client’s explicit consent.
How should therapy notes be stored?
Therapy notes should be stored securely to maintain the confidentiality and integrity of the client’s information. This may involve using locked cabinets or secure digital storage solutions, such as encrypted electronic health record (EHR) systems. It is essential to follow the relevant data protection laws and guidelines in your jurisdiction, such as HIPAA in the United States.
What information should be included in therapy notes?
Therapy notes should include relevant information about the client’s therapy sessions, such as the date, duration, presenting issues, interventions used, the client’s response to those interventions, and any significant events or changes. The level of detail and specific content may vary depending on the type of therapy note (e.g., progress note vs. psychotherapy note). It is essential to maintain a professional, objective tone and adhere to any relevant ethical and legal guidelines.
Can therapists use abbreviations in therapy notes?
Therapists can use abbreviations in therapy notes as long as they are widely accepted and understood within the mental health profession. However, it is essential to ensure that abbreviations do not compromise the clarity or comprehensibility of the notes. If there is any doubt, it’s best to use full terms to avoid confusion or misinterpretation.
Can therapy notes be subpoenaed?
Yes, therapy notes can be subpoenaed under certain circumstances, such as during legal proceedings related to child custody, malpractice claims, or criminal investigations. However, psychotherapy notes are granted a higher level of confidentiality protection and may be less likely to be disclosed compared to progress notes or other types of therapy notes. It is crucial for therapists to understand their ethical and legal obligations in these situations and to consult with an attorney if needed.
Can clients request changes to their therapy notes?
Clients have the right to request changes or amendments to their therapy notes if they believe the information is inaccurate, incomplete, or misleading. Therapists are obligated to consider such requests and determine whether changes are warranted. If the therapist agrees, they should make the necessary changes and inform the client. If the therapist disagrees, they should provide the client with a written explanation of their decision, and the client may have the right to add a statement of disagreement to their record.
How can therapists improve the quality of their therapy notes?
Therapists can improve the quality of their therapy notes by:
- Following a consistent, structured format, such as SOAP or DAP.
- Ensuring that notes are clear, concise, and objective.
- Including relevant and essential information, while avoiding unnecessary details or jargon.
- Writing notes promptly after each session to ensure accuracy and completeness.
- Regularly reviewing and updating notes, particularly treatment plans, to reflect the client’s progress and changing needs.
- Seeking feedback from colleagues or supervisors to identify areas for improvement and enhance professional development.
How do electronic health record (EHR) systems impact therapy notes?
EHR systems have several potential impacts on therapy notes:
Improved efficiency: EHR systems can streamline the process of creating, storing, and managing therapy notes, saving time and reducing administrative burdens.
Enhanced security: EHR systems often provide robust security measures, such as encryption and access controls, to help protect the confidentiality and integrity of therapy notes.
Increased accessibility: EHR systems allow therapists to access therapy notes from various locations and devices, facilitating collaboration and coordination of care with other healthcare providers.
Standardization: EHR systems may offer templates and structured formats for therapy notes, promoting consistency and adherence to professional standards.
Compliance: EHR systems can help therapists maintain compliance with data protection laws and guidelines, such as HIPAA, by providing built-in security features and audit trails.



































![Free Printable Cornell Notes Templates [PDF, Word] 1 Cornell Notes](https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-150x150.jpg 150w, https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-120x120.jpg 120w, https://www.typecalendar.com/wp-content/uploads/2022/05/Cornell-Notes-1200x1200.jpg 1200w)
![Free Printable DAP Notes Templates [PDF & Word] Case Management 2 DAP Note](https://www.typecalendar.com/wp-content/uploads/2023/05/DAP-Note-1-150x150.jpg)
![%100 Free Hoodie Templates [Printable] +PDF 3 Hoodie Template](https://www.typecalendar.com/wp-content/uploads/2023/05/Hoodie-Template-1-150x150.jpg)
