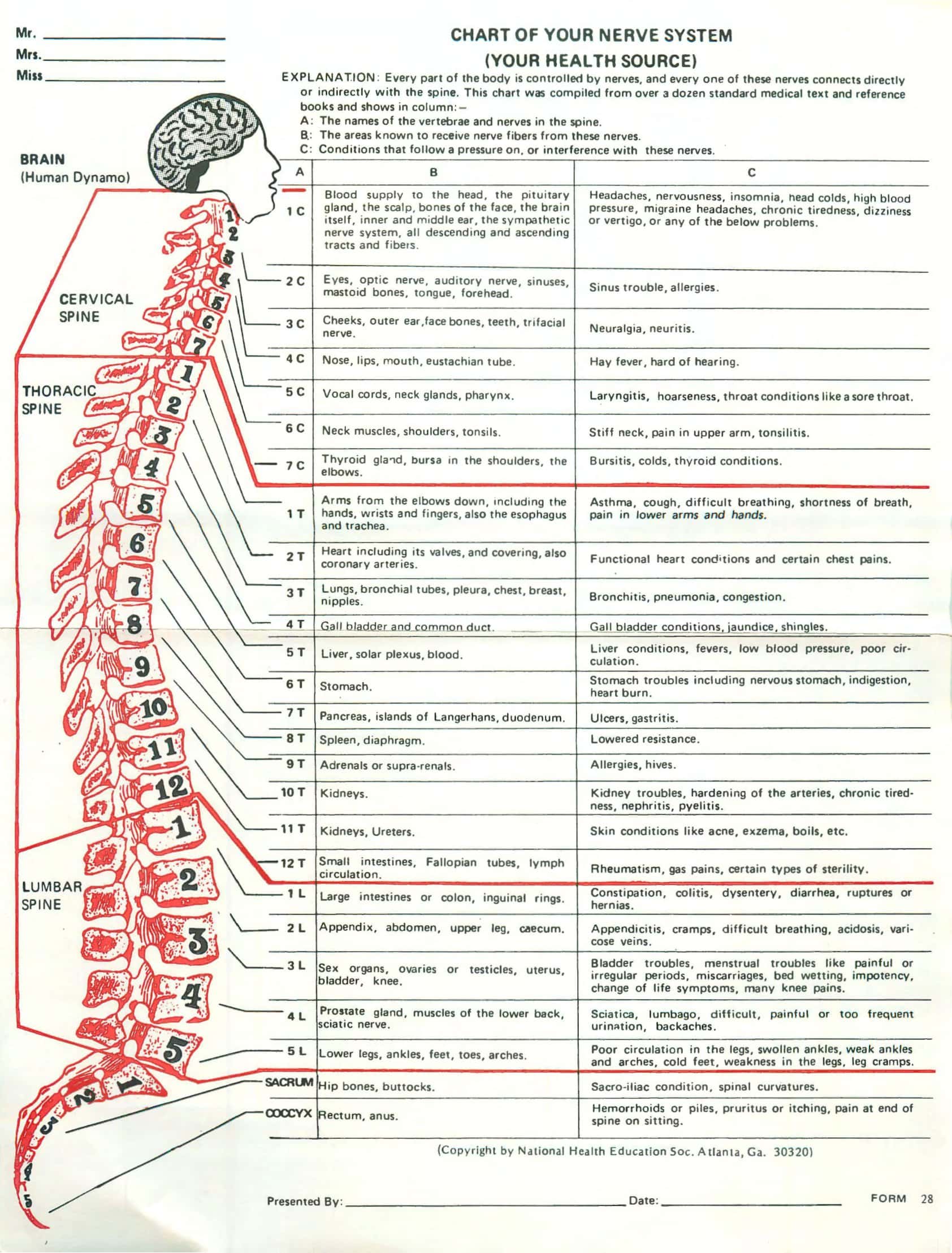
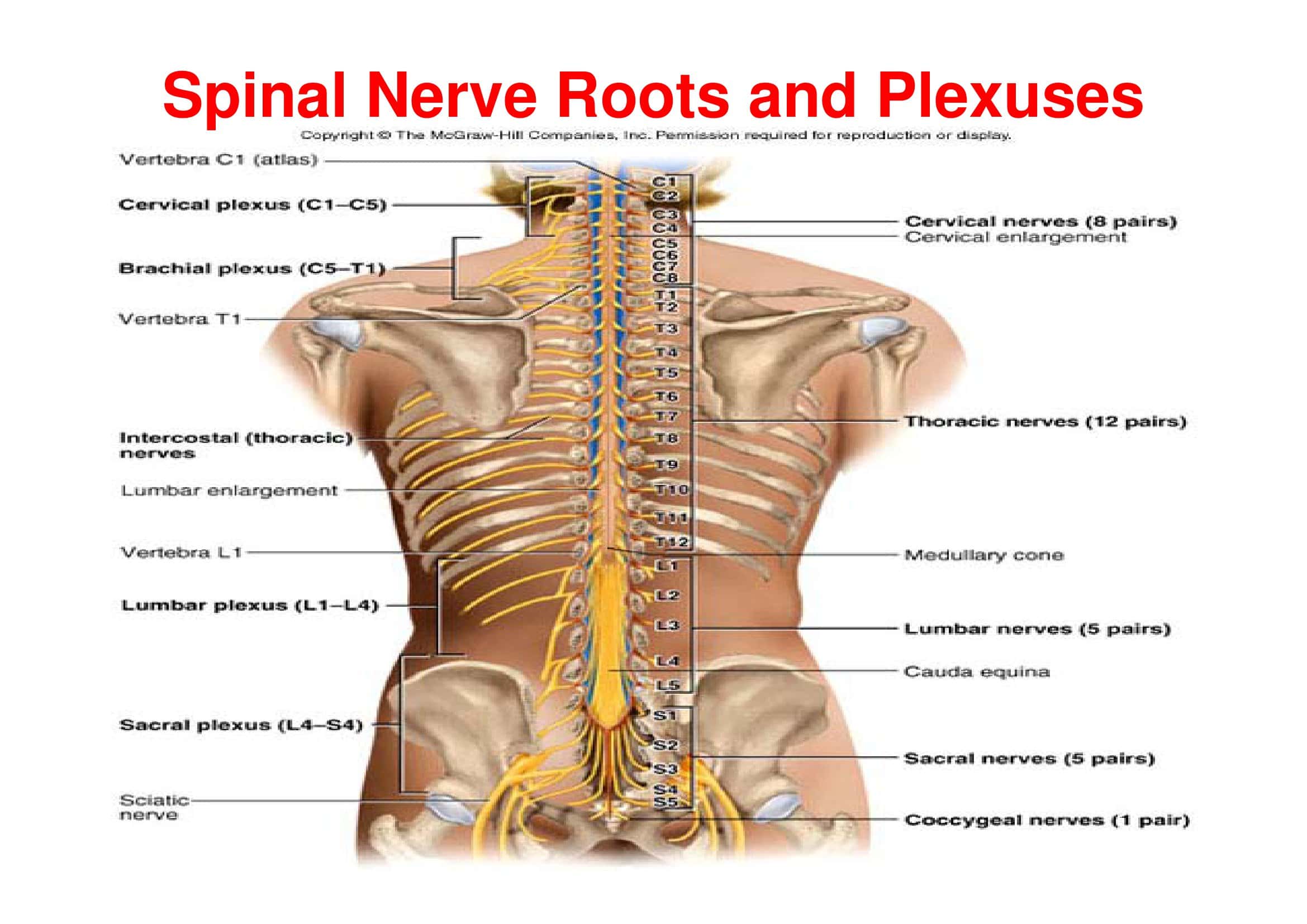
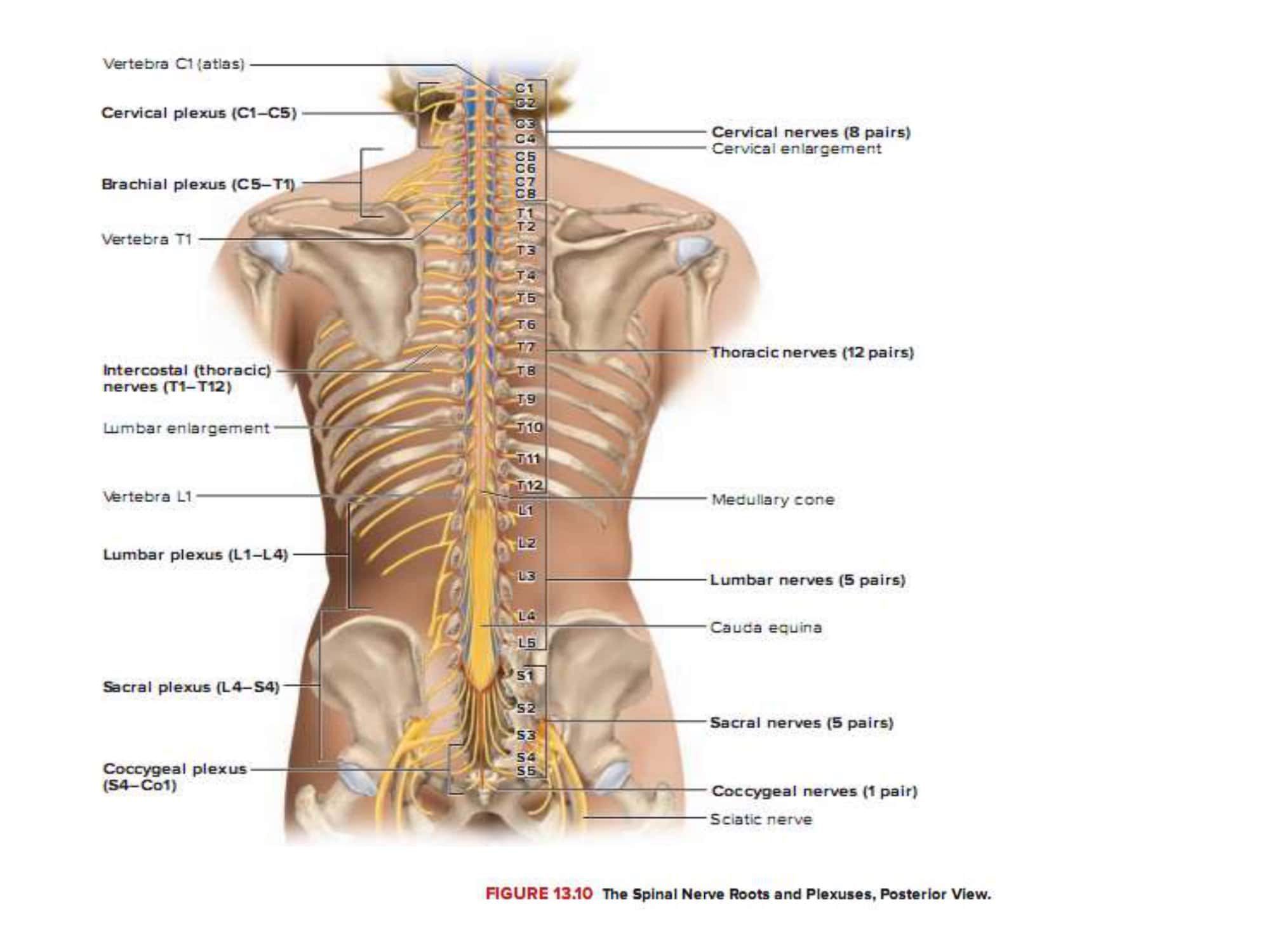
When the clinician shuts the anatomy atlas and hears a patient report tingling along the lateral arm, a vertical grid flashes in his mind: C5, C6, C7. Our Printable Spinal Nerve Chart turns that mental grid into a ready-at-a-glance visual on paper or on any device. From cervical to sacral levels, each segment is more than anatomy—it’s a row of motor commands, sensory zones, and tell-tale clinical signs. That’s why every one of our 30-plus Spinal Nerve Chart templates at TypeCalendar follows the same “vertical logic”: scan top-to-bottom and the segment motor sensory links lock into memory.
Table of Contents
Usage Scenarios — From Exam Room to Study Hall

Quick exam consult: Point to the L5 band on the chart while you reassure the patient—no tangled plexus diagrams required.
High-yield review: Fold the chart and use active recall to hard-code motor actions (C5 abduction, S1 plantar-flexion, and more).
Rehab planning: Highlight exercises by target segment directly on the chart.
Content creation: Drop a low-ink, watermark-free dermatome graphic into blogs or slides with a single click.
Quiz/workshop: Turning the passive look into active production by painting the dermatome boundaries of the students themselves into the blank version.
Printable Spinal Nerve Chart
rom scratch drives the data into long-term storage.
Download Formats & Print Specs
TypeCalendar’s collection of over 30 Printable Spinal Nerve Charts is available in four main file types to ensure a perfect fit for every user. PDF versions (available in A4, US Letter and poster size A3) are ready to be printed on the wall and distributed during the exam, at 300 dpi resolution, so that those searching for “spinal nerve chart PDF download” can access high-quality printouts with one click. Word (.docx) templates are delivered with unlocked layers to meet the needs of “spinal nerve chart Word template”, allowing instructors to add their own notes and clinics to add their institution logos in seconds. Embedding on slides or LMS platforms? Use the PNG with a transparent background and no white borders on dark themes.
Whether you’re looking for a quick free spinal nerve chart download or a high-resolution image to convert into a poster, the right format is waiting for you on one page; all free of charge and without a watermark.
Quick Fire Tips by User Type
Student: Pair the segment strip with the blank outline first; tackle the plexus panel later.
Clinician: Merge the dermatome map and motor table into one laminated PDF for the exam room.
Instructor: Drop three case vignettes into the Word file, then have learners mark the corresponding dermatomes.
Content creator: Nudge the SVG palette toward muted tones, swap the CC line for “Source: TypeCalendar Printable Spinal Nerve Chart,” and embed.
100 % Free, No Watermarks, Ready to Use Templates
All “Printable Spinal Nerve Chart” files are available for free, without watermarks and without a registration wall on TypeCalendar.Choose the layer that suits your needs, download it, customize it according to your use case and turn your vertical spine map into an operational educational tool in a matter of minutes. Discover the collection now to increase learning speed, patient communication and visual clarity.

























![Free Printable Morse Code Charts [Numbers, Alphabet] 1 Morse Code Chart](https://www.typecalendar.com/wp-content/uploads/2023/09/Morse-Code-Chart-150x150.jpg)