In the nexus of healthcare and patient autonomy, the issue of Against Medical Advice (AMA) emerges as a significant point of ethical, legal, and medical concern. When a patient chooses to leave a healthcare facility against the advice of their medical professionals, the outcomes can range from harmless to fatal.
This article delves into the complexities of AMA, exploring its implications for both patient safety and the healthcare system. We will navigate through the reasons why patients opt for AMA, its potential repercussions, as well as the responsibilities and liabilities of healthcare professionals in such scenarios. By investigating these aspects, we aim to foster a nuanced understanding of AMA, enabling informed discussions that respect patient autonomy while promoting optimal healthcare outcomes.
What is an against medical advice form?

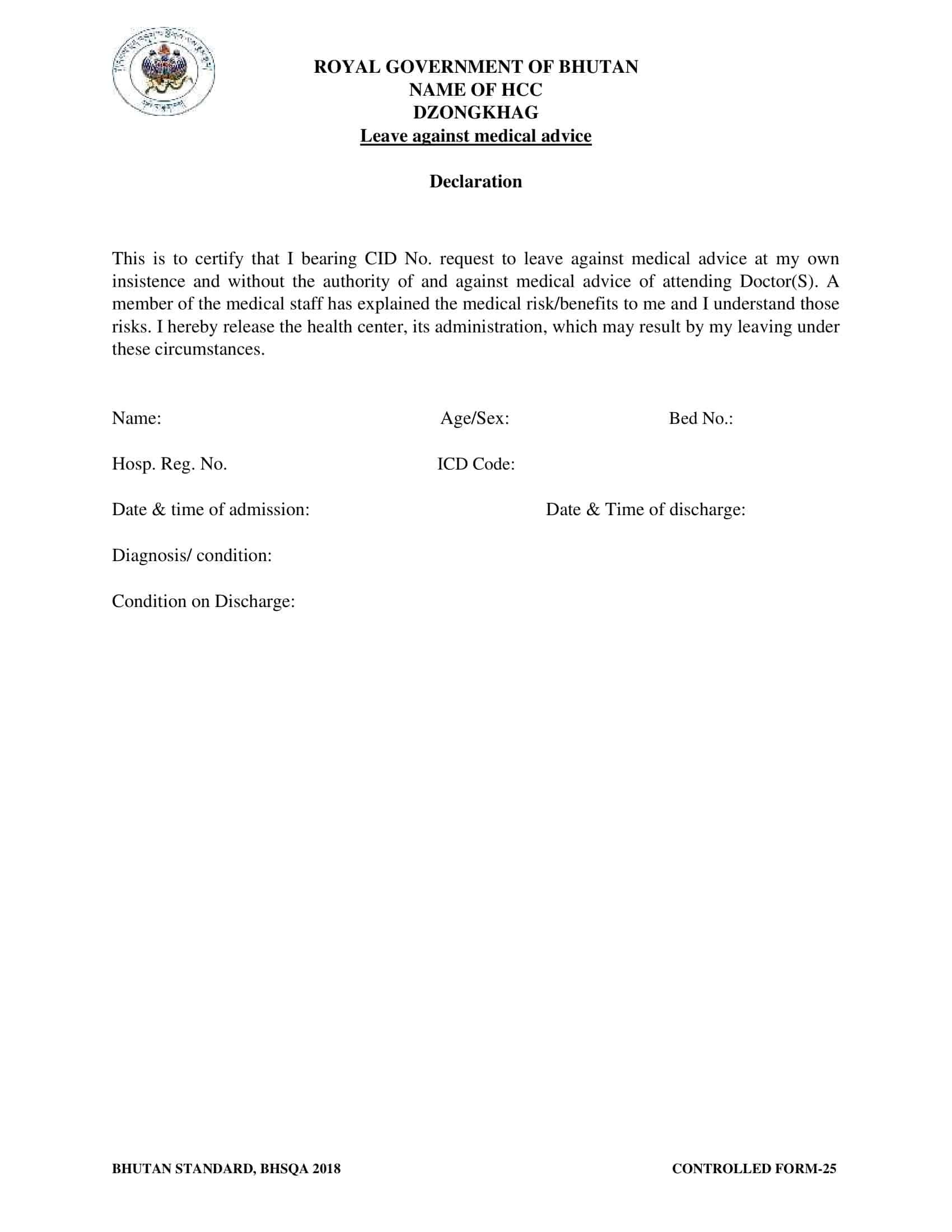
An Against Medical Advice (AMA) form is a legal document used in the healthcare industry when a patient opts to leave a medical facility against the advice of their treating physician. This form primarily serves to confirm that the patient has been adequately informed of their medical condition, potential risks associated with their decision, and possible alternatives, ensuring that their decision is made voluntarily and without coercion.
It acts as a protective measure for healthcare providers against future legal repercussions, documenting that the patient chose to disregard the recommended medical advice. However, it’s important to note that an AMA form does not absolve healthcare professionals from potential liability related to the quality of care provided prior to the patient’s decision.
Table of Contents
Against Medical Advice Form Templates
The purpose of an Against Medical Advice (AMA) form template is to protect both patients and healthcare providers by clearly outlining the risks and potential consequences associated with refusing or discontinuing recommended medical treatments, procedures, or interventions.
These templates typically include fields to capture patient information, such as name, date of birth, and contact details, as well as sections to record the reason for the patient’s decision, discussions held between the patient and the medical team, and any alternative options explored.
A well-designed AMA form template emphasizes clarity and comprehensiveness to ensure that patients fully understand the implications of their decision. It should include detailed information about the specific treatment or procedure being declined, potential risks and complications, and any foreseeable negative outcomes that may arise from non-compliance with medical advice. Additionally, the template should include space for the patient to acknowledge their understanding of the provided information and their agreement to proceed against medical advice.
Why do individuals opt to leave medical care against professional advice?
Patients may choose to leave medical care Against Medical Advice (AMA) for a variety of reasons. Here are some common ones:
Financial Concerns: The cost of treatment can be prohibitive for some individuals, and concerns about medical bills may lead them to leave care prematurely.
Misunderstanding or Lack of Information: Some patients may not fully understand the gravity of their condition or the necessity of the prescribed treatment. They might undervalue the benefits of staying, or overestimate their ability to cope at home.
Personal Obligations: Some patients have responsibilities such as work, childcare, or care for other family members that they believe cannot be put off, leading them to leave care.
Perceived Quality of Care: A patient may leave if they feel dissatisfied with their treatment, or if they have a lack of trust in the competence or attentiveness of the medical staff.
Fear and Anxiety: The hospital environment can be stressful and intimidating, leading to feelings of discomfort or fear, especially among patients with mental health issues or past traumatic experiences.
Substance Use: In some cases, patients with substance use disorders may leave to avoid withdrawal symptoms or to continue using substances.
Leaving AMA: Risks to Patient and Provider
1. Risks to the Patient: The Perilous Path of Self-care
Leaving against medical advice (AMA) carries substantial risks for patients. These risks can be categorized into immediate health risks and long-term health risks.
- Immediate Health Risks: Leaving a medical facility AMA could worsen the patient’s existing condition, lead to complications, or delay recovery. Since patients often do not have the medical expertise to treat themselves, they may fail to recognize and manage complications that arise after discharge.
- Long-Term Health Risks: In the long run, leaving AMA may lead to repeated hospital admissions, a longer overall duration of treatment, and even reduced survival rates in severe cases. Patients may also lose trust in the medical system and avoid seeking medical help in the future, exacerbating their health issues.
2. Risks to the Provider: Legal and Ethical Quandaries
Providers face risks in situations involving patients leaving AMA, too. These primarily take the form of legal risks and impacts on provider-patient relationships.
- Legal Risks: If a patient leaves AMA and suffers harm as a result, the provider may face legal consequences. While an AMA form offers some legal protection, it doesn’t necessarily absolve the provider of all liability. If the patient can prove that the provider didn’t give them adequate information to make an informed decision, or that their condition was improperly managed before they left, the provider might still face legal repercussions.
- Impacts on Provider-Patient Relationships: When a patient decides to leave AMA, it could strain the provider-patient relationship. The patient’s trust in the provider might decrease, affecting future interactions and the patient’s willingness to seek care from that provider. It could also increase stress and dissatisfaction among healthcare providers who are concerned about their patients’ well-being.
What is the AMA process like?
The Against Medical Advice (AMA) process is a complex procedure designed to balance the autonomy of the patient with the ethical and legal responsibilities of the healthcare provider. The aim is to ensure that the patient fully understands the potential risks of leaving medical care and that their decision is made voluntarily.
1. Initial Discussion
Once a patient expresses their intention to leave the facility AMA, the healthcare provider should begin by having an open, non-judgmental conversation with the patient about their concerns and reasons for wanting to leave. This step is crucial for understanding the patient’s perspective and exploring potential solutions that might convince the patient to continue their treatment.
2. Thorough Explanation of Risks
If the patient still wants to leave after the initial discussion, the healthcare provider should then clearly explain the potential medical risks associated with leaving AMA. These might include worsening of the patient’s condition, potential complications, and potential delay in recovery. The healthcare provider should ensure the patient understands these risks.
3. Presentation of Alternatives
The provider should present any reasonable alternatives to leaving. This might include a different treatment plan, palliative care, or even transfer to another facility, if the patient’s concerns are related to their current provider or facility.
4. Documenting the Process
If, after being informed of the risks and alternatives, the patient still chooses to leave AMA, this decision should be thoroughly documented. This documentation is typically done using an AMA form. The provider should document the patient’s mental capacity, the information that was provided to them, their stated reasons for leaving, and the fact that they are leaving against advice.
5. Signing the AMA Form
The patient then signs the AMA form, indicating that they understand and accept the potential risks. If the patient refuses to sign the form, the provider should note this in the medical record. The signing of the form or the refusal to do so should ideally be witnessed by another healthcare worker.
6. Post-AMA Follow-Up
Even after the patient leaves, the provider still has a duty of care. They should provide the patient with instructions for post-discharge care and a clear plan for follow-up, including when and how to seek further medical help if needed.
Can a hospital detain someone against their will?
In general, a hospital cannot legally detain a competent adult patient against their will. Patients have the right to refuse treatment and leave a healthcare facility at any time, even if this decision may negatively impact their health. This right to self-determination is a cornerstone of medical ethics and law, grounded in the principle of patient autonomy.
However, there are certain exceptions where a patient may be detained or held involuntarily in a healthcare setting. These situations typically involve patients who:
1. Lack Capacity
Patients who are mentally incapacitated – due to mental illness, cognitive impairment, or intoxication, for example – may not be legally capable of making informed decisions about their healthcare. If a healthcare professional determines that such a patient lacks the capacity to understand the risks of refusing treatment, they may be held for their own protection until they regain capacity or a legal proxy can make decisions for them.
2. Pose a Threat
In cases where patients pose an immediate danger to themselves or others due to mental health issues, they may be held involuntarily under so-called “involuntary commitment” or “emergency detention” laws. The specifics of these laws vary by jurisdiction, but they generally allow for short-term detention for psychiatric evaluation and possible treatment.
3. Have Contagious Diseases
Some jurisdictions have public health laws allowing for the detention of patients who have certain contagious diseases and refuse treatment, particularly if they pose a risk of spreading the disease to others. This is fairly rare, however.
4. Are Legally Required to Receive Treatment
Certain legal situations may require enforced treatment. One example is when court-ordered treatment is part of a legal judgment or sentence.
- In all these situations, there are specific legal and procedural safeguards in place to protect the rights of the patient, and involuntary detention is generally seen as a last resort. The exact laws and regulations regarding involuntary detention vary by country and state, and healthcare providers must abide by their local regulations.
Is it always unwise to leave against medical advice (AMA)?
The decision to leave Against Medical Advice (AMA) is one that must be made with careful consideration of numerous factors, including the patient’s current health status, the potential risks of leaving, and the individual’s ability to manage their condition outside of a healthcare setting.
In general, medical professionals are trained to provide evidence-based advice, so their recommendations are intended to promote the best possible health outcomes for their patients. Therefore, leaving AMA often has potential risks and may be considered unwise in many situations. However, it’s not universally “unwise” in every circumstance.
Here are a few factors to consider when weighing the decision:
1. Understanding of Medical Condition
Patients should fully understand their medical condition and the potential complications that could arise if they leave early. For example, leaving AMA when the condition is life-threatening or could worsen without immediate care would typically be unwise.
2. Quality of Care
If a patient feels their quality of care is poor or that their concerns are not being addressed appropriately, they might contemplate leaving AMA. In these situations, it may be more beneficial to first communicate these concerns to the healthcare team or consider transferring to a different healthcare provider or facility, if possible.
3. Ability to Self-care or Arrange for Care
Patients who have a support system in place that can help manage their condition outside of a healthcare setting might be in a better position to leave AMA than those who don’t. However, they still need to fully understand their treatment plan and any potential complications.
4. Second Opinion
If a patient disagrees with their current treatment plan, they might think about leaving AMA to seek a second opinion. It’s generally better to do this while still under care, but if that’s not possible, seeking a second opinion after leaving AMA could be a valid course of action, as long as it’s done promptly.
5. Financial Constraints
While financial factors are real and can be constraining, they should be weighed against the potential health risks of leaving AMA. Some hospitals and clinics might offer financial aid, payment plans, or other resources for patients struggling with medical bills.
6. Mental Health
Patients with untreated mental health disorders might make the decision to leave AMA due to fear, anxiety, or confusion. In these cases, it’s crucial that they receive appropriate mental health support.
It’s worth emphasizing that the decision to leave AMA should not be taken lightly. It’s often a good idea for patients to discuss their concerns with their healthcare provider, social workers, or a patient advocate before making a decision. It’s also essential for healthcare providers to listen to their patients’ concerns, explain the potential risks of leaving AMA clearly and comprehensively, and help them make an informed decision that respects their autonomy.
Do’s & Don’ts of AMA: Patients Who Leave Against Medical Advice
Patients who choose to leave a healthcare facility Against Medical Advice (AMA) often do so under complex circumstances. It’s essential for healthcare providers and patients to approach these situations with careful thought and respect for the patient’s autonomy. Here are some key Do’s and Don’ts:
For Patients
Do’s:
- Communicate Openly: Always express your concerns and questions to your healthcare provider. They can provide valuable guidance and may address your concerns, making the thought of leaving AMA less compelling.
- Understand the Risks: Make sure you fully understand the potential risks and consequences of leaving AMA. Ask your healthcare provider to explain any medical jargon or terms that you don’t understand.
- Consider Alternatives: Explore alternatives to leaving AMA, such as a change in treatment plan, a transfer to another facility, or outpatient treatment, if these are viable options.
- Plan for Follow-Up Care: If you decide to leave AMA, have a clear plan for follow-up care. This could include a scheduled visit with your primary care physician, monitoring your symptoms, or knowing when and how to seek emergency care.
Don’ts:
- Don’t Rush Decisions: Avoid making hasty decisions out of frustration or fear. Take the time to fully understand your condition and the potential implications of leaving AMA.
- Don’t Ignore Professional Advice: While it’s your right to make decisions about your own healthcare, it’s generally wise to take the advice of medical professionals into account. They have the training and expertise to guide you toward the best possible health outcomes.
- Don’t Leave Without Documentation: If you leave AMA, ensure you have your medical records or at least a summary of your care. This is essential for any future healthcare provider to understand your medical history.
For Providers
Do’s:
- Listen Actively: Engage in a non-judgmental conversation to understand the patient’s concerns and fears. Sometimes, these conversations can address the issues that are leading a patient to consider leaving AMA.
- Explain Clearly: Provide clear, understandable explanations of the patient’s medical condition, the potential risks of leaving AMA, and any viable alternatives.
- Document Thoroughly: Document every part of the AMA process in detail, from the patient’s capacity to make decisions, the discussions that took place, to the information provided about potential risks and the patient’s understanding of those risks.
Don’ts:
- Don’t Force the Patient: Respect the patient’s autonomy. Although you might disagree with their decision, it’s their right to decide as long as they have the capacity to do so.
- Don’t Neglect Follow-Up Care: Even if a patient leaves AMA, provide instructions for self-care at home and encourage them to seek follow-up care. Their decision to leave does not absolve healthcare providers of their duty of care.
- Don’t Make Assumptions: Each patient’s situation is unique. Avoid making assumptions about why they want to leave AMA, and instead engage in open dialogue to understand their specific circumstances.
Sample “Leaving AMA” Documentation
Patient: John Doe
MRN: 123456
Date: June 20, 2023
Time: 14:30
Note Type: Against Medical Advice (AMA) Documentation
Clinical Background: The patient, Mr. John Doe, was admitted to the hospital on June 18, 2023, with a diagnosis of community-acquired pneumonia. He has been receiving IV antibiotics and supportive care. His condition has been improving but requires further treatment and observation.
AMA Process:
Patient’s Decision: At approximately 13:45 today, Mr. Doe expressed a desire to leave the hospital due to personal reasons, specifically citing concerns about missing work.
Discussion with Patient: I engaged in a detailed conversation with Mr. Doe regarding his concerns. We discussed potential alternatives, such as a later discharge time or potential coverage options for missed work. However, Mr. Doe maintained his decision to leave immediately.
Capacity Assessment: A mental status examination was conducted to assess Mr. Doe’s capacity to make an informed decision. Mr. Doe was alert and oriented to person, place, time, and situation, demonstrating adequate decision-making capacity.
Explanation of Risks: The potential risks of leaving AMA were discussed at length with Mr. Doe. These include the risk of his pneumonia worsening, potential complications, and the need for readmission. Mr. Doe acknowledged understanding these risks.
Alternatives and Benefits: We discussed continuing inpatient treatment until complete resolution of the pneumonia and the benefits of a full course of antibiotics in a controlled environment. Despite this, Mr. Doe insisted on leaving.
AMA Form: The AMA form was presented to Mr. Doe, outlining the risks and benefits of his decision. He read the form and signed it. This was witnessed by Nurse Jane Smith.
Discharge Instructions: Despite his decision to leave AMA, Mr. Doe was provided with discharge instructions, including signs and symptoms that should prompt immediate medical attention, a prescription for oral antibiotics, and instructions to follow up with his primary care provider in two days.
Summary: Mr. Doe decided to leave the hospital against medical advice. The potential risks and benefits of this decision were thoroughly explained, and he demonstrated understanding of these. The decision was made voluntarily and without coercion.
Provider: Dr. XYZ, MD
FAQs
What information does an Against Medical Advice form typically include?
An AMA form usually includes the patient’s identifying information (name, date of birth, etc.), the reason for the patient’s decision to leave against medical advice, a statement indicating that the patient understands the potential risks and consequences of their decision, and a section for the patient’s signature, indicating their informed consent.
Can an Against Medical Advice form be revoked or reversed?
Once a patient has signed an Against Medical Advice form, it is generally considered legally binding. However, it is advisable for patients to have a conversation with their healthcare provider if they have second thoughts or concerns about their decision. Depending on the circumstances, healthcare providers may be able to address the patient’s concerns, provide additional information, or recommend alternative options.
Can insurance coverage be affected if a patient leaves against medical advice?
Insurance coverage can be affected if a patient leaves against medical advice. Insurance companies may deny or limit coverage for medical expenses related to the condition for which the patient refused recommended treatment. It is crucial to review the insurance policy and consult with the insurance provider to understand how leaving against medical advice may impact coverage.
Can healthcare providers refuse treatment if a patient wants to leave against medical advice?
Healthcare providers generally have the right to refuse further treatment if a patient chooses to leave against medical advice. However, they are still obligated to provide necessary emergency care until the patient’s condition stabilizes or until another healthcare provider assumes responsibility for the patient’s care.
Are there any legal requirements for an Against Medical Advice form?
Legal requirements for an Against Medical Advice form may vary depending on jurisdiction. It is important to consult with local healthcare regulations or legal professionals to understand any specific requirements in your area. Generally, the form should include clear and concise information about the patient’s decision, the risks involved, and the patient’s acknowledgment of those risks.
Can family members or caregivers override a patient’s decision to leave against medical advice?
In general, family members or caregivers do not have the authority to override a patient’s decision to leave against medical advice unless they have legal guardianship or power of attorney for medical decisions. However, healthcare providers may consider the input of family members or caregivers in discussions with the patient and provide them with information to help them understand the potential risks and consequences.
Can leaving against medical advice impact future medical care?
Leaving against medical advice can potentially impact future medical care. Some healthcare providers may be hesitant to provide care to patients who have previously left against medical advice, as they may perceive them as non-compliant or at higher risk for adverse outcomes. It is important to maintain open communication with healthcare providers and address any concerns or questions they may have regarding your previous decisions.







































![%100 Free Hoodie Templates [Printable] +PDF 1 Hoodie Template](https://www.typecalendar.com/wp-content/uploads/2023/05/Hoodie-Template-1-150x150.jpg)
![Free Printable Medical Health History Form Templates [PDF] Example 2 Medical Health History Form](https://www.typecalendar.com/wp-content/uploads/2023/05/Medical-Health-History-Form-1-150x150.jpg)
![Free Printable Food Diary Templates [Word, Excel, PDF] 3 Food Diary](https://www.typecalendar.com/wp-content/uploads/2023/05/Food-Diary-1-150x150.jpg 150w, https://www.typecalendar.com/wp-content/uploads/2023/05/Food-Diary-1-1200x1200.jpg 1200w)
